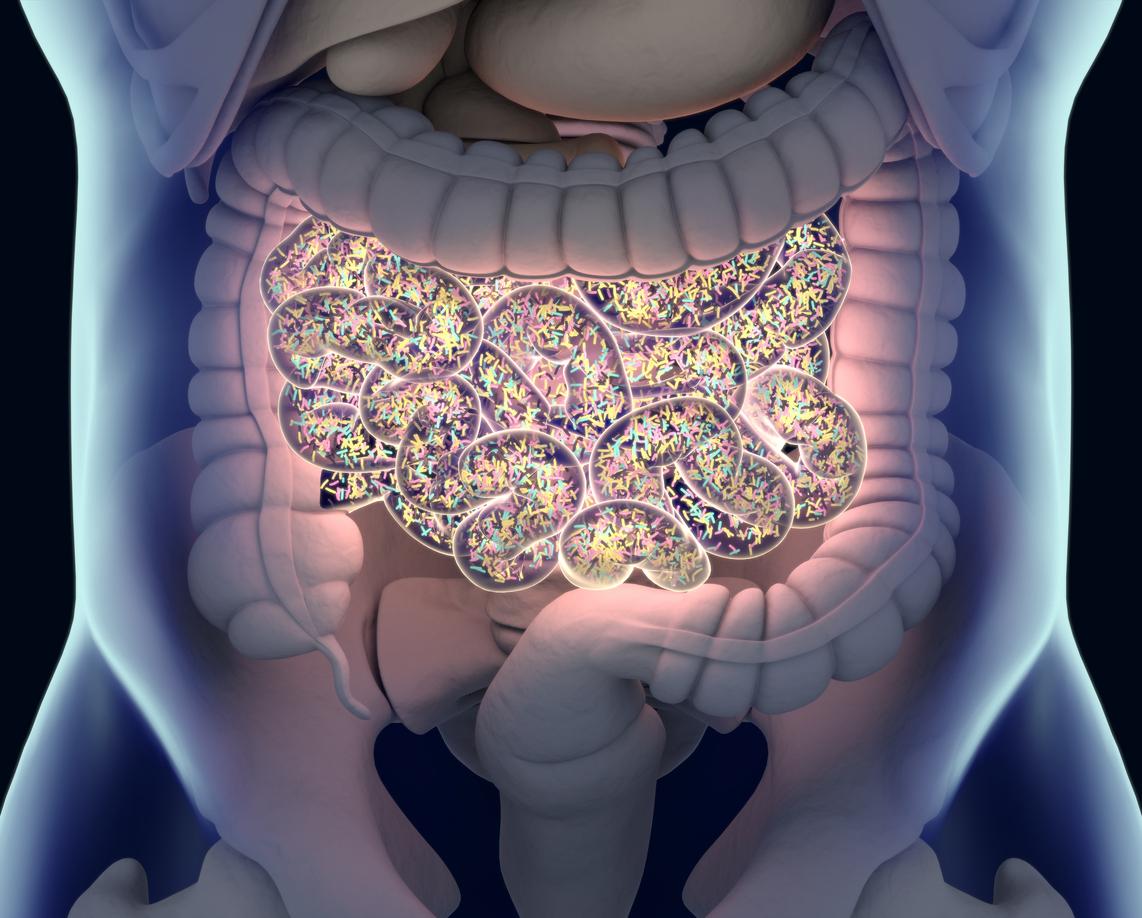
An observational study of patients in Finland and the Netherlands suggests gut microbiota composition may be linked to risk of hospitalization for infection.
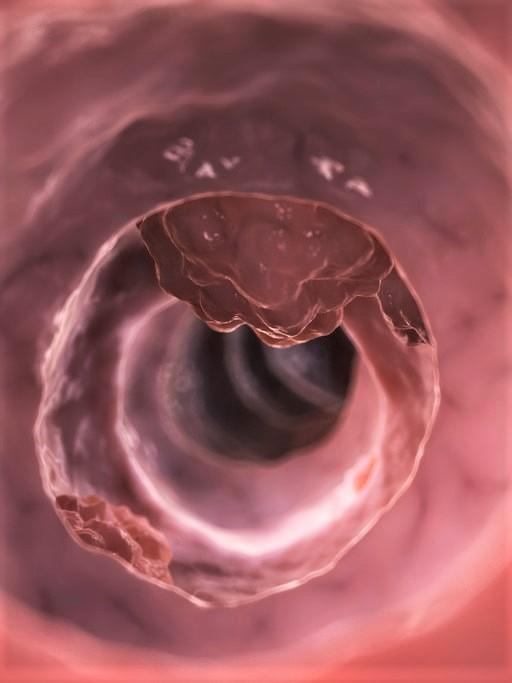
In the study, which was released last week in advance of the upcoming European Congress of Clinical Microbiology and Infectious Diseases, a team led by researchers at Amsterdam University Medical Center sequenced the DNA of fecal samples from 10,699 participants (4,248 from the Netherlands and 6,451 from Finland). Their aim was to measure the microbiota composition, diversity, and relative abundance of butyrate-producing bacteria—which are commonly depleted in patients hospitalized for severe infections—and examine associations with infection risk using computer modeling. Pre-clinical models have indicated butyrate-producing bacteria may have a protective effect against systemic infections.
Over 5 to 7 years of follow-up, 602 study participants were hospitalized with or died from infections, mainly community-acquired pneumonia, and the researchers found that their gut microbiota composition differed from those who were not hospitalized. Specifically, each 10% increase in abundance of butyrate-producing bacteria was associated with a 25% reduced risk of hospitalization in the Dutch participants and 14% lower risk in the Finnish cohort. These associations remained unchanged after adjustment for demographics, lifestyle, antibiotic exposure, and comorbidities.
"Gut microbiome composition, specifically colonisation with butyrate-producing bacteria, is associated with protection against hospitalisation for infectious diseases in the general population across two independent European cohorts," the study authors wrote. "Further studies should investigate whether modulation of the microbiome can reduce the risk of severe infections."