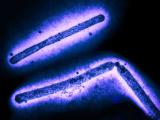
Federal and state health officials today reported that a person connected to a dairy farm in Texas has tested positive for H5N1 avian flu, the first known case linked to sick dairy cows and the nation's second since the virus began circulating in wild bird and poultry in 2022.
Today's case announcement underscores new interim guidance that the Centers for Disease Control and Prevention (CDC) released over the weekend on preventing, detecting, and responding to avian flu infections in humans, which are very rare and mainly pose a threat to people who are exposed to sick animals or contaminated environments.
The day before the CDC posted its new guidance, the US Department of Agriculture (USDA) Animal and Plant Health Inspection Service announced that highly pathogenic avian influenza (HPAI) has now been confirmed in a dairy herd in Michigan, bringing the number of affected states to five.
Eye redness the only symptom
The CDC said today that the patient reported eye redness (conjunctivitis) as the only symptom and is recovering. The patient has been asked to isolate and is being treated with a flu antiviral drug.
The Texas Department of State Health Services (TDSHS) said the person had contact with dairy cows, and it urged healthcare providers to be vigilant for people with symptoms of H5N1 flu, especially in those who have close contact with animals that have suspected infections.
Though conjunctivitis isn't a common symptom of seasonal flu, the TDSHS said it has been seen before in people infected with avian flu viruses.
In its new guidance, the CDC urged people exposed to H5N1 in birds or other animals to monitor themselves for new respiratory symptoms, including conjunctivitis, for 10 days following initial exposure. The monitoring is recommended even for people who wear recommended personal protective equipment.
For patients with conjunctivitis symptoms, the CDC recommends that healthcare providers obtain both conjunctival and nasopharyngeal swab samples.
"CDC is working with state health departments to continue to monitor workers who may have been in contact with infected or potentially infected birds/animals and test those people who develop symptoms," the agency said in its news release today.
Current H5N1 clade can cause a range of illnesses
Past experience with H5N1 suggests that people who have contact with sick animals are at highest risk. The CDC and its state partners routinely monitor people exposed to the virus, and from January 2022 through September 2023—a period when the US poultry industry was hit hard by the virus—had monitored about 6,500 people from 52 jurisdictions.
Of those, illnesses were reported in 165 people, and of those, testing revealed H5N1 in only 1, a person who was involved with culling at a poultry farm in Colorado. Fatigue was the man's only symptom. Asymptomatic cases were reported in a few poultry workers in the United Kingdom and Spain who were positive for H5N1 in initial tests, and it's not clear if their results reflected true infection or surface contamination of the upper airway tract.
The H5N1 clade circulating in the United States and several parts of the world, however, has resulted in severe and fatal infections. Globally, at least 12 cases involving the 2.3.4.4b H5N1 clade have been reported, according to CDC background data. The disease was fatal in a patient in China, and Chileans and Ecuadorians had critical illnesses. Nearly all had been exposed to sick or dead birds.
An older H5N1 clade circulating in parts of Asia has been linked to a spate of recent H5N1 infections in Cambodia, most of which were severe or fatal. The cases typically involved people who had exposure to sick poultry.
Federal and state officials in the United States emphasize that the overall risk to the public is very low. With strong safeguards in place for the commercial milk supply, including routine pasteurization, they have repeated their longstanding assertion that raw milk can harbor pathogens and pose serious health risks to consumers.
Michigan findings add evidence of cow-to-cow spread
APHIS said the Michigan dairy herd had recently received cows from Texas, where the virus had already been confirmed. "Spread of symptoms among the Michigan herd also indicates that HPAI transmission between cattle cannot be ruled out," the group said. Similarly, Idaho's agriculture department last week announced that HPAI was detected at a facility that had imported cattle from an earlier-affected state.
The Michigan Department of Agriculture and Rural Development said the dairy herd where HPAI was found is in Montcalm County, which is in the central part of the state. The cattle were moved from Texas before any animals on the source farm showed signs of disease, and they didn't have any symptoms or appear ill when they were moved to Michigan.
Genetic sequencing suggests that the H5N1 virus found in Michigan is very similar to strains confirmed in Texas and Kansas and was probably initially introduced to the dairy herds by wild birds, according to APHIS. So far, sequencing shows no changes in the virus that would make it more transmissible to humans.