A randomized controlled trial in Hong Kong finds that the synbiotic drug SIM01 relieves multiple symptoms of long COVID, or post-acute COVID-19 syndrome (PACS).
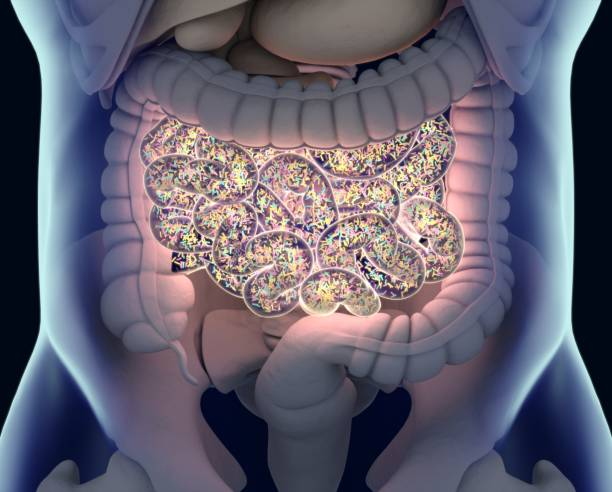
SIM01 contains strains of anaerobic Bifidobacterium bacteria (which are probiotics) and soluble fibers (prebiotics) to alter the gut microbiome and possibly modify immune response.
Twice-daily doses
From June 2021 to August 2022, researchers from the Chinese University of Hong Kong randomly assigned 463 adult long-COVID patients at a single hospital in a 1:1 ratio to receive SIM01 or a vitamin C placebo by mouth twice daily for 6 months. The median interval between infection and random assignment was 4 months.
The investigators clinically assessed participants at baseline for symptoms, quality of life, and physical activity level. At 6 months, interviewers administered a 14-item symptom questionnaire to participants and collected blood and fecal samples to assess changes in the gut microbiome and blood cytokines (small proteins that trigger the immune response).
"Decreased abundance of short-chain fatty acid-producing bacteria in the gut of patients with COVID-19 might represent one of the crucial mechanisms contributing to the gut–lung interaction and thereby disease severity in COVID-19," the researchers wrote.
The study was published yesterday in The Lancet Infectious Diseases.
No effect on quality of life, exercise ability
Nearly one third of patients (31%) had been hospitalized during their infections. At 6 months, significantly higher proportions of the SIM01 group reported an improvement in fatigue (odds ratio [OR], 2.27), memory loss (OR, 1.97), difficulty concentrating (OR, 2.64), gastrointestinal upset (OR, 2.00), and general unwellness (OR, 2.36) than the placebo group.
Decreased abundance of short-chain fatty acid-producing bacteria in the gut of patients with COVID-19 might represent one of the crucial mechanisms contributing to the gut–lung interaction and thereby disease severity in COVID-19.
Increases in relative benefit after SIM01 therapy were 47% for fatigue, 56% for memory loss, 62% for difficulty concentrating, 30% for gastrointestinal upset, and 31% for general unwellness.
Rates of adverse events were similar between the two groups (SIM01, 10% vs placebo, 11%), and none were considered related to treatment. Receipt of SIM01, infection with Omicron subvariants, vaccination before COVID-19 infection, and mild COVID-19 infection were predictors of symptom improvement.
Average visual analog quality-of-life scores (on a scale of 0 to 100) at 6 months weren't significantly different (76.0 for SIM01 recipients vs 74.5 for the placebo group). Nor was there a significant difference in physical activity at 6 months, per total metabolic equivalent of task-minutes per week (SIM01 median, 1,646.3 vs placebo, 1,902.0).
Symptom relief tied to certain microbiome changes
Fecal metagenomic analyses showed that the gut microbiome was more diverse, including more short-chain acid-producing bacteria and fewer genes related to antibiotic resistance, at 6 months than at baseline in SIM01 recipients but not the placebo group.
Correlation of microbial changes with symptoms showed that relief of specific symptoms was tied to distinct compositional and functional changes in the microbiome.
"For instance, Bifidobacterium adolescentis showed positive correlations with alleviation in fatigue, gastrointestinal upset, and memory loss," the researchers wrote. "We also found that alleviation in fatigue and general unwellness correlated with an elevated relative abundance of Bifidobacterium bifidum, whereas alleviation in difficulty in concentration correlated with a positive shift in Bifidobacterium longum."
Cytokine analyses yielded no significant results.
"Treatment with SIM01 alleviates multiple symptoms of PACS," they wrote. "Our findings have implications on the management of PACS through gut microbiome modulation. Further studies are warranted to explore the beneficial effects of SIM01 in other chronic or post-infection conditions."
Lack of universal long-COVID symptom assessment tool
In a related commentary, Betty Raman, DPhil, and Maheshi Ramasamy, DPhil, both of the University of Oxford, said that emerging evidence points to the importance of the gut microbiome in the development of long COVID, with a disruption in microbial balance, or gut dysbiosis, in some patients.
"There are now several studies showing that probiotics, consisting of beneficial bacteria such as Lactobacillus and Bifidobacterium species, might enhance gut health, modulate inflammation, and improve immune function," they wrote.
The real benefits of the treatment on general health perception and functional capacity might be low.
But study limitations such as the lack of a universally accepted long-COVID symptom assessment tool and a reliance on subjective symptom reports complicates interpretation of the findings.
"Although alleviation of some symptoms of PACS was observed, this alleviation did not correspond with measurable improvements in quality of life or physical activity after 6 months, suggesting that the real benefits of the treatment on general health perception and functional capacity might be low," Raman and Ramasamy wrote.