- An international research consortium that specializes in human-challenge studies has announced the launch of a $57 million project to test inhaled and nasal vaccines with a goal of stopping infection from SARS-CoV-2 and other coronaviruses, the Coalition for Epidemic Preparedness Innovations (CEPI) announced yesterday. The project is led by Imperial College London and is cofounded by the European Union's Horizon Union Programme and CEPI.
- China has reported another human infection involving H9N2 avian flu, the first of 2024, according to a weekly avian flu update from Hong Kong's Centre for Health Protection. The patient is a 6-year-old boy from Anhui province whose symptoms began on January 3. The report did not say how the child contracted the virus. H9N2 infections are typically mild and reported in children. The virus is known to circulate in poultry in some Asian countries.
- The New Mexico Department of Health last week reported a fatal plague case, which involves a man from Lincoln County who had been hospitalized. The infection is the state's first since 2021, and the man's death is the first plague-related fatality since 2020. Rodents can harbor the plague bacterium, Yersinia pestis. The disease can spread to humans through bites from infected fleas or from direct contact with animals, including rodents, wildlife, and pets.
Quick takes: Next-gen coronavirus vaccines, H9N2 avian flu case in China, fatal plague in New Mexico
Pneumococcal vaccines may protect against viral respiratory infections, study finds
In addition to preventing pneumococcal disease, pneumococcal conjugate vaccines (PCVs) are associated with some protection against viral respiratory tract infections (RTIs), according to a systematic literature review published yesterday in the Journal of Infectious Diseases.

The review, conducted by researchers with Pfizer and Belgian research company P95, looked at observational and interventional studies published from 2000 through 2022 on the vaccine efficacy (VE) and overall effect of the PCV7, PCV9, PCV10, or PCV13 vaccines against viral RTIs. Given the synergistic interactions between viral and bacterial pathogens and the hypothesis that the effectiveness of PCVs against all-cause pneumonia might be linked to reduction of viral-associated pneumonia episodes, the researchers wanted to evaluate the evidence on the effects PCV against virus-related RTIs in children and adults.
Of the 16 studies that were included in the final analysis, 13 described the effects of PCVs against viral RTIs in children and 3 included data on adults. In children, data from 4 studies showed VE against influenza ranged from 41% to 86%, except for the 2010-2011 flu season, and a randomized controlled trial showed PCV9 displayed efficacy against any viral RTI, human seasonal coronavirus, parainfluenza, and human metapneumovirus. In adults, PCV13 VE ranged from 4% to 25% against viral lower RTI, 32% to 35% against COVID-19 outcomes, 24% to 51% against human seasonal coronavirus, and 13% to 36% against influenza A lower RTI.
No protection was found against adenovirus or rhinovirus in children or adults.
Broader public health benefits
The study authors say the simplest explanation is that PCVs are preventing pneumococcal-viral coinfections. But they also suggest that the vaccines, by influencing pneumococcal carriage in the upper airway, may modify host susceptibility to viral lower RTIs. They say further research is needed to confirm the findings and to further explore the clinical benefits and broader public health impacts of PCVs at a population level.
They concluded, "If results from studies conducted to date are corroborated, PCV protection against RTIs beyond those due to pneumococci might better capture the full spectrum of public health benefits of PCVs, thereby informing vaccine policymaking and economic evaluations."
Study finds racial, ethnic disparities in broad-spectrum antibiotics in kids

A single-center study of children hospitalized with acute respiratory infections found that children in certain racial and ethnic groups were more likely to receive broad-spectrum antibiotics than White children, researchers reported late last week in the Journal of the Pediatric Infectious Diseases Society.
For the retrospective cohort study, researchers from the University of Washington, Seattle Children's Research Institute, and Seattle Children's Hospital analyzed all patients aged 18 years and younger hospitalized with respiratory illnesses at Seattle Children's Hospital from October 2020 to April 2023. While studies conducted in pediatric emergency department settings have identified racial disparities in antibiotic prescribing, prescribing disparities in pediatric inpatient settings have not been well documented. The primary outcome of the study was any antibiotic use and any use of broad-spectrum antibiotics.
Of the 1,779 patients included in the analysis, roughly half received at least one dose of a systemic antibiotic, with no statistically significant difference in antibiotic receipt by racial or ethnic group. But in an adjusted analysis that excluded children with conditions that generally warrant antibiotics, Asian children were nearly five times as likely (adjusted odds ratio [aOR], 4.92; 95% confidence interval [CI], 1.35 to 17.9) to receive broad-spectrum antibiotics when compared with non-Hispanic White children.
When the analysis was further adjusted to remove intensive care unit admission and insurance, Asian children (aOR, 1.63; 95% CI, 0.94 to 2.85) remained more likely than non-Hispanic White children to receive broad-spectrum antibiotics, along with Hispanic (aOR, 1.97; 95% 1.24 to 3.13), non-Hispanic Black (aOR, 2.49; 95% CI, 1.16 to 5.36), and unknown/other (aOR, 1.77; 95% CI, 1.08 to 3.13) children.
No reason for disparities in prescribing
The authors say the findings are surprising, since studies conducted in ambulatory settings have generally found that Black and Hispanic children are less likely to receive antibiotics for viral respiratory tract infections and bronchitis than White children. Furthermore, there's no biological or medical reason for differences across racial and ethnic groups.
"Further research is needed to identify the factors driving these disparities and to develop strategies that ensure equitable and effective antibiotic utilization practices by pediatric providers," they wrote.
Estimated risk of mpox hospitalization 4% in UK epidemic, with higher risk in women
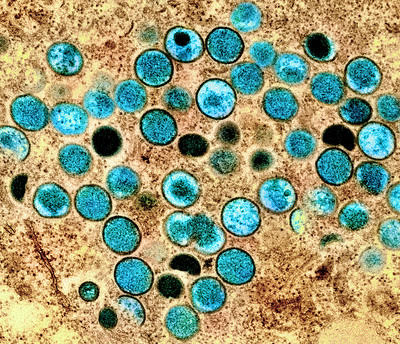
In a study of UK mpox patients in 2022, the risk of hospitalization was 4% overall, with a much higher risk in women than in men that could be due to increased disease severity or lower illness detection in women, the researchers said.
The investigators, from the UK Health Security Agency in London, published the results yesterday in Nature Communications.
In the 2022 epidemic, mpox was first detected in the United Kingdom on May 7, followed by rapid transmission around the world. In July, the World Health Organization declared the primarily sexually transmitted infection, which spread mainly among men who have sex with men, a public health emergency of international concern.
'Considerable' uncertainty about risk in women
A total of 3,375 UK residents tested positive for mpox from June to September, with an estimated 74.7% case capture. The estimated modeled risk of hospitalization was 4.1%, while the overall sample case hospitalization risk was 5.1%. The average time from infection to hospitalization was 14.9 days, and the average length of hospital stay was 7.1 days.
For women, the estimated sample case hospitalization risk was 17.9%, compared with 5.0% for men. "However, there is considerable uncertainty due to the small number of female cases in the clinical and surveillance data," the study authors wrote.
The team called for ongoing public health surveillance to limit the healthcare burden in affected countries.












