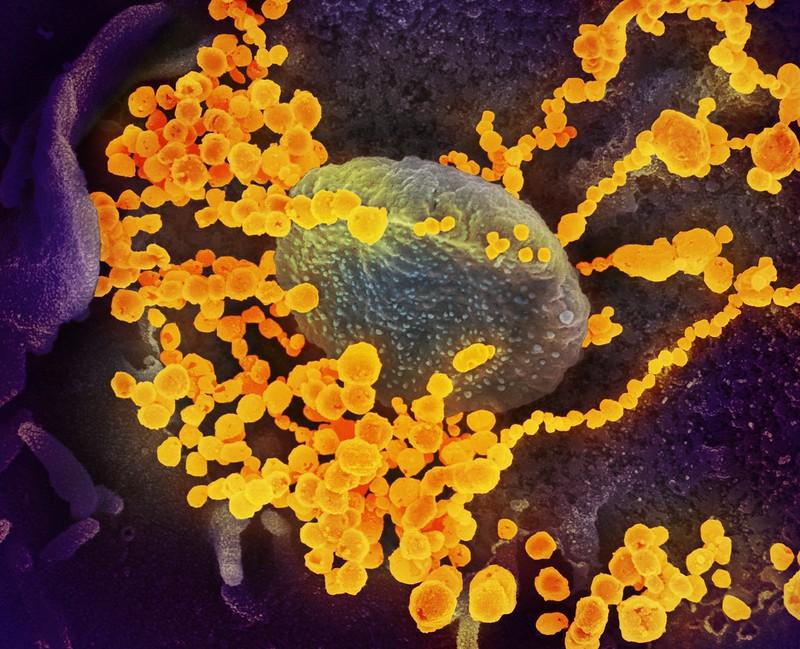
A common genetic mutation may be why some people have COVID-19 but have no symptoms, according to a University of California, San Francisco (UCSF)–led study published yesterday in Nature.
The researchers noted that at least 20% of people with COVID-19 infections never feel ill. "Although most global efforts have focused on severe illness in COVID-19, examining asymptomatic infection provides a unique opportunity to consider early immunological features that promote rapid viral clearance," they wrote.
The team, which also included scientists from La Trobe University in Australia, other US researchers, and a UK scientist, enrolled 29,947 people with high-resolution human leukocyte antigen (HLA) genotyping data in a smartphone-based study to monitor COVID-19 symptoms and outcomes from February 2020 to April 2021. They also analyzed cells from those with the HLA9-B*15:01 genetic variant who donated blood several years before the pandemic.
The researchers hypothesized that an HLA mutation may be the reason some infected people are able to dodge COVID-19 symptoms by quickly eradicating the virus. The study focused on 1,428 unvaccinated people who tested positive for SARS-CoV-2.
HLA genes code for proteins that the immune system uses to identify healthy cells and those infected with bacteria or viruses.
Immune system primed to recognize SARS-CoV-2
Of the 29,947 participants, 136 (0.45%) were asymptomatic for at least 2 weeks before and after a positive result. Testing two independent groups for a link between five genomic HLA locations with disease course revealed a strong relationship between HLA-B*15:01 and asymptomatic infection.
This mutation, found in about 10% of the population, was detected in 20% of study participants who never became sick, compared with 9% of their ill counterparts. Participants who carried two copies of the genetic variant were more than eight times more likely to have no symptoms. Risk factors for severe COVID-19 (eg, older age, presence of chronic diseases such as diabetes) didn't appear to affect asymptomatic status.
It’s like having an army that already knows what to look for and can tell by the uniform that these are the bad guys.
People with the mutation had memory T cells (a type of white blood cell) against a certain SARS-CoV-2 particle. In other words, those who were unexposed to SARS-CoV-2 had previous exposure to similar viruses and had developed immunologic memory against that particle.
Virus eliminated before symptoms developed
"We hypothesized that their immune system could react so fast and powerfully that the virus was eliminated before causing any symptoms," co-senior author Jill Hollenbach, PhD, of UCSF, said in a University of North Carolina news release. "It’s like having an army that already knows what to look for and can tell by the uniform that these are the bad guys."
Most reactive T cells had a memory phenotype, were multifunctional, and were cross-reactive to a peptide derived from seasonal coronaviruses. "So, even if the bad guys changed the uniform, the army would still be able to identify them by their boots or maybe a tattoo on their arms," Danillo Augusto, PhD, of the University of North Carolina, said in the release. "That is how our immunological memory works to keep us healthy."
Studying immune responses "might enable us to identify new ways of promoting immune protection against SARS-CoV-2 that could be used in future development of vaccine or drugs," co-senior author Stephanie Gras, PhD, of La Trobe University, said a UCSF news release.