"What's going on?"
—Marvin Gaye
"If you don't know where you're going, any road will get you there."
—Lewis Carol
"It ain't over till it's over."
—Yogi Berra
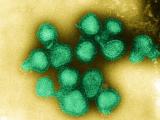
(CIDRAP Business Source Osterholm Briefing) – As much as we'd all like to put behind us the tale of H1N1, the first influenza pandemic of this century, I'm afraid it's too soon to stamp the words "The End." What's more, I've reached a conclusion that the way we define severity—or lack thereof—is as antiquated as the egg technology we've used to produce a vaccine for 40-plus years.
Just whom do you believe?
If you are confused about the "state of the novel H1N1 pandemic," don't feel alone. The past few weeks have seen a variety of media reports, scientific publications, and blog posts that support, or at least imply, the conclusion that the current influenza pandemic is likely the "mildest on record" and seems to be waning. You might also have seen stories asserting that such public health agencies as the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC) have had evidence that this was a mild pandemic months ago and yet have continued to hype its seriousness.
But if you look at written reports and statements from these same international and federal health agencies, you'll find they have made the case that this pandemic has extracted a severe price, particularly among children and younger adults, is far from over, and that it's critical to get as many people as possible vaccinated as soon as possible.
So does anyone really know what is going on or where this H1N1 pandemic road is going to take us?
I’ll try to give you some context and suggest rational next steps. I've spent every day since this novel H1N1 pandemic was recognized critically analyzing data, looking to extract the straight story that I can share with you. I'll start with a brief summary of our pandemic trip to date and where I think we could be going over the next several months.
Trying to predict the next steps of a virus like H1N1 is always risky. But if you look back over the last 7 months of columns, I think you'll find we've been largely on the mark about how this virus might behave, the availability of an effective vaccine, and how government and organizations would respond.
Three critical questions should be front and center for you, your family, and your organization:
- Has this pandemic to date been a big deal or has this been a bunch of hype? Or maybe it's been somewhere in between?
- Where are we in this pandemic experience? Is it over—or is another big "shoe" about to drop?
- If it's not over, what should you be doing for yourself and your family to be better prepared, and what should your organization be doing?
Big deal or a bunch of hype?
Without a doubt, this pandemic has been a big deal worldwide if you, a loved one, or a member of your organization has been seriously ill, even worse if you've lost someone to the disease or its complications. Just last Thursday the CDC updated its estimated number of H1N1-related US cases and deaths. As of November 14:
- Approximately 9,820 people have died (estimated range, 7,070 to 13,930)
- More than 47 million people have been infected with H1N1 (range, 34 million to 67 million)
- Some 213,000 persons have been hospitalized (range, 154,000 to 303,000)
Of note, this recent analysis captures much of the impact of the second wave of H1N1 that we saw this fall. Just a month ago the CDC released illness and death estimates through October 17, a period that largely preceded the fall wave, and the number of cases and deaths were substantially lower. I congratulate CDC's experts on the work they've done to arrive at these illness, hospitalization, and mortality estimates. From my epidemiologic perspective, they used a credible and thoughtful method.
But, I must admit that it's hard for most of us to take numbers like this and make a meaningful conclusion about the seriousness of the pandemic. It's a lot like automobile accidents; the annual fatality statistics mean little to us until it includes someone you know or love.
Of course, there is one number that we often hear, especially when people try to compare the impact of the H1N1 pandemic to seasonal influenza. It's usually cited this way: "Approximately 36,000 people in the US die each year from seasonal flu." Its source is a single 2003 CDC modeling paper. In short, this seems like a no-brainer: 9,820 people have died from H1N1 to date and we expect 36,000 to die annually from seasonal influenza. Yep, this pandemic is a lot of hype!
Wait, hold on. It's not that simple. Let's provide some perspective behind the 36,000 figure:
- Comparing apples to oranges. In that CDC study, only 9,000 of those estimated annual seasonal deaths are due directly to influenza or secondary bacterial pneumonia. The other deaths are among persons who have influenza and who die of events like heart attacks or strokes. If you want a comparison, think of the guy who has a heart attack while snow blowing his driveway after a large snowstorm and whose death is labeled "storm-related."
- The elderly. More than 90% of the estimated seasonal influenza deaths occur in the elderly, who in many instances have existing serious health conditions that mean their deaths may not be far off, regardless of their influenza illness. We all realize that death is inevitable, and, as a public health practitioner, I find that this mad race to eliminate the top 10 causes of death is not always well thought through. If we were to accomplish such a goal, there would be 10 new leading causes of death, and I'm not so sure some of those would be better than the current ones. But I think we can all agree that "early deaths"—or those that occur well before our elderly years —just shouldn't happen. The way we count influenza mortality, an influenza-related death in an 87-year-old person with advanced Alzheimer disease is the same as the death of a 22-year-old otherwise perfectly healthy pregnant woman. Both deaths are equally tragic, but any reasonable person would agree they are not equivalent public health outcomes.
How can we measure the pandemic impact today?
Let's take a closer look at the numbers of deaths associated with the H1N1 pandemic. Of the estimated 9,820 deaths:
- 1,090 (11%) have occurred in children 0-17 years of age
- 7,450 (76%) in people 18-64 years of age
- 1,280 (13%) in people over 65 years of age
This age distribution differs considerably from what we see with seasonal influenza.
To truly describe the impact of this pandemic, we need to apply the concept of years of potential life lost[75] (YPLL[75]), which is an estimate of the average years a person would have lived if he or she had not died before 75 years of age. As such, it is a measure of premature mortality that gives more weight to deaths that occur among younger people (including people likely to be in your workforce and their children).
While I have not seen a calculation estimating the YPLL[75] for either the H1N1 pandemic or a typical seasonal influenza season, it is clear the current pandemic to date far dwarfs seasonal influenza in this important measure. And as I'll describe in more detail below, there may be a lot more H1N1 illnesses and deaths to come.
Another comparison that is very important is how the current H1N1 pandemic compares to past pandemics. If we look at the rate of deaths in the US population from novel H1N1 through November 14, the 9,820 deaths among the US population of 308 million translates to a figure of 0.003% (or 32 deaths per million population). (See table below.) The rate of deaths per age-group varies this way:
- 14.9 deaths per million children 0 to 17 years of age
- 38.9 deaths per million adults 18 to 64 years of age
- 33.0 deaths per million adults 65 years of age and older.
If we look at deaths for the dreaded 1918 pandemic, the estimates range from 500,000 to 750,000 deaths among a population of 100 million (0.5 to 0.75% or 5,000 to 7,500 per million). While there remains some ambiguity in the 1918 death numbers and how they were determined, they are at least 150 times higher than what we've seen to date with the H1N1 pandemic. Like the current pandemic, the 1918 deaths occurred at a much higher rate in young adults. We all have to be thankful that a repeat of 1918 has not occurred with this current pandemic. Imagine our world right now if that were happening.
Number of estimated US deaths per million
for influenza pandemics in the last century
Year Rate per million population1918-19
5,000 to 7,500
1957-58
407
1968-69
170
2009-10 (as of Nov. 14)
32
Similarly, when we look at the 1957-58 and 1968-69 pandemics, death rates are substantially higher than we have documented to date with novel H1N1.
- In the 1957-58 pandemic, an estimated 70,000 deaths occurred among 172 million US residents (407 per million).
- In the 1968-69 pandemic, an estimated 34,000 deaths occurred among 200 million US residents (170 per million). Like seasonal influenza, many of the deaths in both of these two pandemics occurred in the elderly population. In other words, they were more like "super-seasonal influenza" years.
Two other pieces of important data were notable in the CDC's H1N1 update last week. To date, the pandemic has caused:
- More cases than seasonal influenza. To date, we know of an estimated 47 million cases of novel H1N1. That's already 16 million more than the estimated 31 million cases that occur during an average seasonal influenza year. We are still ascertaining the level of workplace absenteeism associated with the increased illnesses and the need to find child care as a result of nearly 2,000 school closings this fall that affected 616,000 students, according to the CDC.
- More hospitalizations than seasonal influenza. An estimated 213,000 hospitalizations to date have been related to H1N1 illness. That number exceeds by 13,000 the estimated average seasonal influenza year of 200,000 hospitalizations.
As I've noted before, we're still a long way from being done with this pandemic; a third wave during the traditional winter flu months is still a possibility. Also, as I've noted in previous columns, the impact of these cases on the healthcare system has been dramatic.
During the Southern Hemisphere's recent winter influenza season (June-August), Australia and New Zealand experienced a 1,500% increase in admissions to their intensive care units (ICUs) compared with a regular flu season. Many of the severely ill cases of H1N1 infection among the younger population require intensive care that is rarely needed among the elderly with seasonal influenza.
While I don't know of any US hospitals that have reached the tipping point with increased ICU admissions, I do know many that have been severely challenged. I just spoke with an ICU physician at a Midwest pediatric hospital who said the fall of 2009 presented the greatest challenge of her 25-year career. She dreaded the thought of what the upcoming winter months would bring. The good news is that, because of the availability of the modern ICU—something not available in previous pandemics—the number of critically ill patients who have been saved has made a difference in the overall number of pandemic-related deaths. But if a serious third wave occurs, there is no promise that some of these ICUs won't be overrun.
So yes, this current pandemic is causing fewer deaths than the three previous ones, particularly compared with 1918. Still, this pandemic is causing a marked increase in deaths in younger adults and children compared with a typical seasonal influenza year. It's challenging our healthcare system unlike any previous seasonal influenza season over the past 30 years. That makes it hard for me to call this a "mild” pandemic. I just don't believe the term works.
Yes, there are mild, moderate, or severe influenza illnesses on an individual basis. But how do we describe a pandemic that hits a limited group of people really hard and causes only "routine influenza" for most others?
It's like saying for any given year we can classify our collective automobile accidents as mild, moderate, or severe. That just doesn't work. Most accidents are nothing more than minor fender benders with no injuries. Surely these are "mild" events. We might call "moderate" those collisions that result in serious, but non-life-threatening injuries. And surely we'd call collisions with fatalities "serious."
But just as we don't call the sum of the annual automobile accidents by one descriptive term, we must find a better way to talk about and compare influenza pandemics. Maybe it should be on a YPLL[75] scale of high, medium, or low. On this type of scale, this pandemic is one of consequence—it's more than just mild!
Where are we in this pandemic experience?
The past 2 weeks I have read an increasing number of news stories and blog postings that sound like obituaries for the novel H1N1 pandemic of 2009. These stories naturally gravitated to the point I mentioned earlier that somehow public health agencies hyped just how severe this pandemic would be. In short, I believe these agencies did the only responsible thing they could do—they provided all the possibilities that a pandemic might bring.
So, does the rapidly waning second wave, which began in North America in mid-August, mean the end of the pandemic? I don't think so. As Mark Twain once said, "The reports of my death are greatly exaggerated." Unfortunately, I believe the same is true for this novel H1N1 pandemic. If you've seen one pandemic, you've seen one pandemic. No one knows what Mother Nature and this virus will do. But just look at the numbers:
- Infection. The estimated 47 million cases of H1N1 infection to date means that only 15% (47 million/308 million) of US residents have immune protection from an H1N1 infection.
- Vaccination. Last week, the CDC reported about 73 million doses of vaccine have been shipped to the states. And while more vaccine is coming, my sense is that demand is dropping faster than the US stock market in 2008. I believe this is due in part to (1) the perception of some that the waning second wave means the pandemic is over, (2) busy schedules during the holiday season, and (3) the belief that there is now enough vaccine, so if anyone needs it in the future, they can simply get it at their convenience. And of course, there is that approximate 50% of the US population that has reported in multiple polls that they will not take the vaccine for themselves or have their children vaccinated out of a false concern (my words, not theirs) about vaccine safety. If even 75 million Americans get vaccinated, that represents only 25% of the population.
- Existing immunity. Given that there appears to be some residual acquired immunity in people over 65 years of age and who were exposed to a "cousin" of the current H1N1 virus before the 1950s, we can add on a guesstimate of another 10% to 15% of that population who have existing immunity.
When you add up the percentages of the three ways people can be protected against this novel H1N1 virus, we find that almost half of all residents in the US are still susceptible to infection and will be come this January. In countries where there is no or limited vaccine access, the percentage of citizens not yet protected will be even higher.
Given these numbers, I can't think of any good reason why we won't have a serious third wave of disease in the Northern Hemisphere during this upcoming traditional winter influenza season.
Just last week we got some sobering news from the American College Health Association that speaks to this issue. After weeks of decline, H1N1 influenza activity on US college campuses increased 27% from the previous week among students returning after the Thanksgiving break. And for weeks the number of students vaccinated has hardly budged. It remains at about 5%. I'll be very interested to see what happens on these campuses after the winter break. Remember, the fall second wave really got started after students returned to school (elementary, junior high, high school, technical, and college) this past August. Will we see a repeat of that in January? If I were a betting man, I wouldn't bet against it.
So, while I hope I'm wrong, we may have to go through the drill again with H1N1 this winter. I do believe that if H1N1 illness picks up, then substantially more people will seek vaccine. But because of limited distribution locations and trained personnel, mass vaccination won't happen overnight—even if the vaccine is available. And remember, adults need probably at least 7 to 10 days after vaccination before they will have any protection—even longer for kids under 10 years of age, who need two doses.
And two last footnotes. First, I've not said anything about the occurrence of seasonal influenza. In the 1957 and 1969 pandemics, previous seasonal flu strains virtually disappeared during the pandemic waves. But will that occur in the winter of 2009-10? I don't have a clue. But if even some seasonal influenza occurs, it will only complicate our response capacity.
Second, if the novel H1N1 virus undergoes reassortment or a critical mutation in the next weeks to months, it could really complicate our lives, particularly if it diminishes the effectiveness of our current vaccine or results in the widespread transmission of an H1N1 virus resistant to the antiviral drugs we are currently using.
What should you and your organization do now?
The first and most important step to remember is this: vaccine, vaccine, and vaccine. Despite the downturn in cases and reduced media attention to the level of illness in our communities, get everyone you love, know, work with, or spend time with to the vaccine line as soon as possible. I'm certain that in the next 2 weeks vaccine supplies will free up substantially, and in most communities anyone will be able to relatively easily find a dose of vaccine. Don't let the busy holiday season hold you back, either. The best protection for the third wave will be vaccine.
As for your organization, go back over what you learned about the impact that the fall wave had on your operations. Given what you learned, what can you reasonably do to be better prepared for a similar, if not more significant, winter wave? And if that wave doesn't materialize, you wasted little. This H1N1 virus may be the predominant seasonal flu strain for years to come, so you'll not waste your time or a vaccine dose if you get it now. And of course the preparedness work you do now to collect and respond to lessons learned during the fall wave will be used some day in the future, even if only for the next pandemic.
Bottom line for your organization
"What's going on?"
This current H1N1 pandemic is surely not of a magnitude of the 1918 pandemic, or even the 1957 or 1969 pandemics. But it is a serious public health threat, and it's far from over. Expect the unexpected! That's the flu business.
"If you don't know where you're going, any road will get you there."
We must focus our efforts on getting as many of our loved ones, colleagues, and friends vaccinated as vaccine supplies become more abundant. This will be the most important road we can take right now. Continue to review and update your pandemic preparedness plans. You may have little time to do this later this winter.
"It ain't over till it's over."
Get ready: This could be a challenging winter. Do not write the H1N1 pandemic obituary yet. In fact, this lull after the second Northern Hemisphere wave is our time to regroup. If only a limited third wave occurs, your efforts will still be of great value. If a doozy of a third wave occurs, you will have been prescient in your efforts.