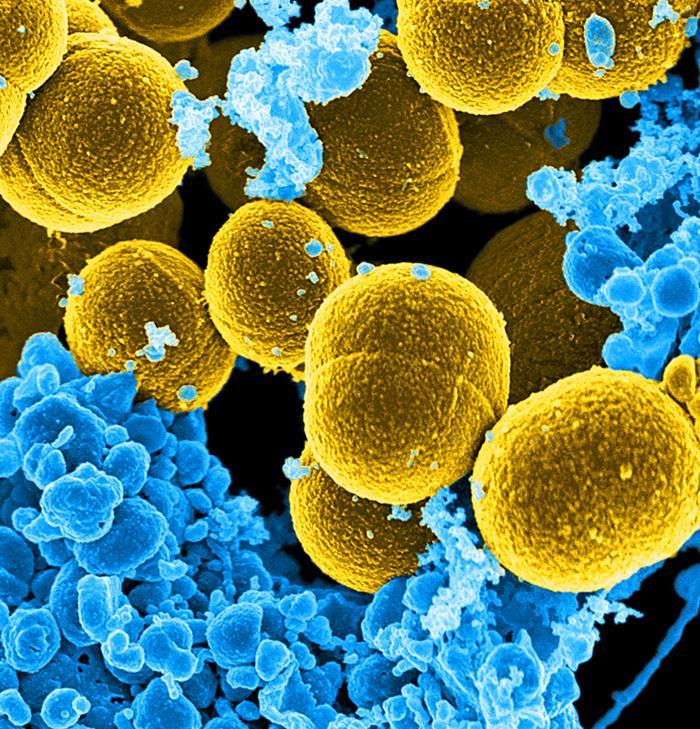
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections in children has decreased over the past decade, as it has in adults, while overall susceptibility to antibiotic treatments has varied in this age-group, researchers from the San Antonio Military Medical Center found.
Changes to antibiotic prescribing practices in children are probably unwarranted, therefore, according to an expert commenting on the study.
Study included 39,000 kids
The study authors, whose findings were published yesterday in Pediatrics, evaluated lab records of 41,745 S aureus isolates obtained from 39,207 pediatric patients hospitalized within the US Military Health System from 2005 to 2014. MRSA was defined as resistance to cefoxitin, methicillin, or oxacillin.
Over the 10-year period, S aureus showed an overall trend of increased susceptibility to erythromycin, gentamicin, and oxacillin and decreased susceptibility to clindamycin, ciprofloxacin, and TMP.SMX [trimethoprim-sulfamethoxazole].
For example, susceptibility to oxacillin increased by 14.8%, from 59.4% to 68.4%, while susceptibility to clindamycin decreased from 90.7% to 86%.
S aureus infections showed modest increases in susceptibility to non–beta lactam antibiotics, with a 6% recent increase for ciprofloxacin (74.5% in 2011 and 80% in 2014), and a rise for erythromycin over the 10-year period from42.1% to 49.7%. Susceptibility to erythromycin increased, although more than half of isolates remained erythromycin-resistant.
When the researchers compared antibiotic susceptibility of MRSA and methicillin-susceptible S aureus (MSSA) infections, they found that 90.5% of MRSA infections remained susceptible to clindamycin, while MSSA clindamycin susceptibility declined from 90.7% to 83.8% during the decade. MRSA susceptibility to erythromycin increased from 12.1% to 20.5%. MSSA infections had a 34.8% higher rate of susceptibility to ciprofloxacin than did MRSA infections.
Most pediatric S aureus cases (32,222) were skin and soft-tissue infections (SSTIs), which were significantly less susceptible to oxacillin than were respiratory or sterile site infections (P < 0.0001), though SSTI oxacillin susceptibility rose slightly over the decade from 53.9% to 65.5%.
Oxacillin susceptibility also varied by age-group and geographic region. Children aged 1 through 5 years were significantly less susceptible to oxacillin compared with other age-groups (51.6% susceptible; P < 0.0001). Oxacillin susceptibility also rose significantly between 2011 and 2014 throughout most of the United States, with notable increases of 16.3% in the Midwest and 14.3% in the South.
The investigators said rates of MRSA in children seem to be declining, as they have for adults during the past several years. They recommend that, given apparent decreases in susceptibility of S aureus to clindamycin, physicians be aware of potential resistance when prescribing the antibiotic to pediatric patients.
Changing Staph epidemiology
In a related commentary in the same issue of Pediatrics, Sheldon L. Kaplan, MD, of Texas Children's Hospital, notes that changes to pediatric empiric antibiotic prescribing practices are not currently warranted, referencing recent observations on the decline of healthcare-acquired invasive MRSA and stable rates of community-acquired S aureus in pediatric patients.
"The epidemiology of S aureus infections in children has been changing over the past 2 decades," he said, "which is why it is critical to keep a very close eye on this common pathogen."
See also:
Mar 1 Pediatrics study
Mar 1 Pediatrics commentary