In an unusual trial reported yesterday, the use of two different experimental Ebola vaccines in different prime-boost sequences appeared safe and induced detectable immune responses in a small group of volunteers, though one vaccine generated a much stronger initial response than the other.
And in another Ebola development, an experimental Ebola drug called TKM 130803 failed to improve survival in very sick Ebola patients in a Sierra Leone trial, according to a report yesterday in PLoS Medicine. The researchers held out hope that the product might still prove helpful in patients with less severe illness.
Two different vectors used
The phase 1 vaccine trial, described in the Journal of the American Medical Association (JAMA), involved vaccines called Ad26.ZEBOV, developed by Crucell Holland B.V., and MVA-BN-Filo, made by Bavarian Nordic. They are two of several Ebola vaccines currently in development. No Ebola vaccine has yet been licensed, but the vaccine known as VSV-EBOV worked well in a field trial in Guinea in 2015 and is now used to respond to Ebola flare-ups.
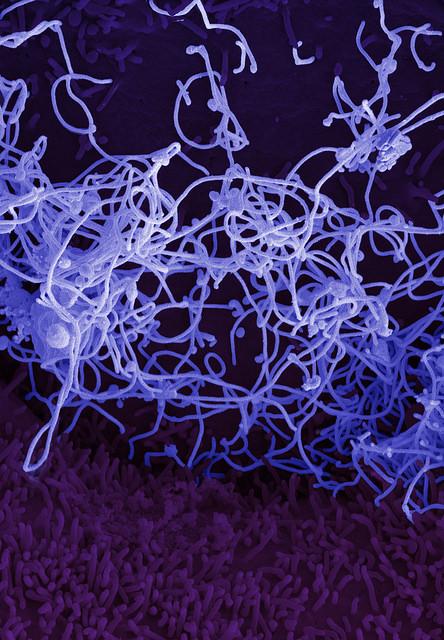
Ad26.ZEBOV, like two other Ebola vaccines, uses an adenovirus to carry genetic material from the Zaire Ebola virus, the strain that caused West Africa's epidemic.
MVA-BN-Filo employs modified vaccinia Ankara (MVA), a weakened form of vaccinia virus (which is used in smallpox vaccines) to deliver the same Ebola component. The virus also carries material from Sudan Ebolavirus, Tai Forest Ebolavirus, and the related Marburg virus, according to the National Institute of Allergy and infectious Diseases (NIAID), which has supported work on both vaccines.
The vaccines were tested in a randomized controlled trial launched in December 2014 at Oxford University in the United Kingdom, involving healthy adults ages 18 through 50. The basic approach involved giving one vaccine as a prime dose and using the other one as a booster.
The researchers enrolled 87 volunteers, with a median age of 38.5 years; 66.7% were women. Seventy-two participants were randomly divided into four groups of 18. At the start, 3 in each group received a placebo vaccine, and the other 15 received an injection of either Ad26.ZEBOV or MVA-BN-Filo, the NIAID said in a press release. Participants then received a booster dose with the other vaccine or a second placebo either 28 or 56 days later.
A fifth group of 15 volunteers enrolled in an open-label group received the Ad26.ZEBOV vaccine on day 1. Of this group, 12 received the MVA-BN-Filo vaccine 14 days later, while the other three participants received no booster shot.
Findings on safety and immunogenicity
With safety and tolerability as the primary trial outcomes, the researchers reported no serious vaccine-related adverse events. Three of 60 (5%) Ad26.ZEBOV recipients in the four randomized groups experienced a fever, as did 4 of 15 in the open-label group, whereas none of the MVA-BN-Filo recipients had a fever, the report says.
The most common side effect was injection-site pain, generally mild to moderate, the researchers said.
The immune responses to the first doses of the two vaccines differed sharply. In the randomized groups, 28 of 29 Ad26.ZEBOV vaccinees (97%; 95% confidence interval [CI], 82%-99.9%) had detectable Ebola-specific antibodies (IgG) 28 days after the initial dose, versus 7 of 30 MVA-BN-Filo recipients (23%; 95% CI, 10%-42%). Among the Ad26.ZBOV vaccinees, 55% also showed T-cell responses.
But this contrast in immune responses decreased after the booster doses. All the vaccinees had Ebola antibodies detectable 21 days after the booster injection and when checked again at 8 months, according to the report. In addition, at least 86% of those in the randomized groups showed Ebola-specific T-cell responses at 1 week after the booster shot. The T-cell responses also persisted at 8 months, the report says.
Partial protection called likely with one dose
"Our data showed that, in contrast to MVA-BN-Filo, Ad26.ZEBOV priming generated an initial immune response, and there is evidence for protection from this vaccine given alone in nonhuman primate models," the researchers wrote. "Therefore, this priming dose would be expected to generate at least partial protection against Ebola; for this reason, Ad26.ZEBOV prime schedules with MVA-BN-Filo boost are currently being further evaluated in phase 1, 2, and 3 studies."
The NIAID said the "durable protection" seen in the trial "could prove important in areas with intermittent outbreaks of Ebola, in order to provide baseline protection for the community."
The study authors commented that the low response to MVA-BN-Filo as the prime dose might limit that vaccine's use in an Ebola outbreak situation. "However, the postboost antibody and T-cell responses appear robust in these groups, and these schedules merit further study. Additional immunization schedules using priming with the MVA-BN-Filo vaccine are being evaluated in a separate phase 1 study and will further inform the potential role for this approach."
The report mentions a previous study in which MVA-BN-Filo was used as a booster after a prime dose of another Ebola vaccine, ChAd3. That study, published in January in The Lancet Infectious Diseases, suggested that such a regimen could confer long-lasting protection.
The investigators also wrote that the persistence of humoral and cellular immune responses for 8 months with their prime-boost regimen might offer an advantage over a single-dose vaccination strategy, especially in circumstances in which long-lasting protection is more important than fast protection.
As for limitations of the study, they said it is unclear whether preexisting immunity to the adenovirus vector could limit immune responses to the Ad26.ZEBOV vaccine. Very few volunteers in their trial had Ad26 antibodies, they noted, but one previous report suggested that 40% to 60% of sub-Saharan Africans could have low to moderate antibody levels against Ad26. "The issue will be addressed in ongoing phase 1 and 2 studies," they wrote.
Ebola drug fails to increase survival
Meanwhile, the use of the experimental drug TKM-130803 failed to help Ebola patients in a trial at a clinic in Port Loko, Sierra Leone, according to the PLoS Medicine report.
The drug interferes with the production of two essential Ebola virus proteins and has been shown to improve survival in monkeys experimentally infected with Ebola virus, said a press release from Oxford University. Scientists from Oxford and Sierra Leone worked with several other groups on the trial.
In the phase 2 trial, funded by the Wellcome Trust, adults with confirmed Ebola virus disease received intravenous doses of TKM-130803 once daily for up to 7 days. On days when trial enrollment capacity was reached, patients were enrolled in an observational cohort. The primary outcome was survival to day 14 after admission, excluding patients who died within 48 hours of admission.
The predetermined "futility boundary" for the study was reached after 14 patients had been treated with the drug, the report says. Two patients died within 2 days of admission and were excluded from the analysis. Of the other 12, 9 died and 3 survived. Two of three patients who were enrolled in the observational group also died.
"Most of the patients entering the Ebola Treatment Centre at the time the study was enrolling, which included those given TKM-130803, had very severe Ebola disease, so further studies are needed to assess if the drug might provide a benefit in patients with less severe disease," the press release states.
"The drug was well tolerated by all of the patients and we've learnt a lot about giving the drug to patients with Ebola," senior author Peter Horby, MBBS, PhD, commented in the release. "Once we get the results of on-going tests of the drug concentration in the patients' blood we will have a better understanding of the optimal dose for any further studies."
Milligan ID, Gibani MM, Sewell R, et al. Safety and Immunogenicity of novel adenovirus type 26–and Modified Vaccinia Ankara–vectored Ebola vaccines: a randomized clinical trial. JAMA 2016 Apr 19;315(15) [Abstract]
See also:
Apr 19 NIAID press release
Apr 19 PLOS Medicine report
Apr 19 University of Oxford press release
January 2016 Lancet Infect Dis study involving ChAd3 vaccine with MVA-BN-Filo as booster