In two new major Ebola virus developments, an international expert group has proposed guidance for post-exposure prophylaxis, and what may be the most in-depth analysis of blood samples from sick patients revealed markers that provide new clues about how the disease unfolds and which patients are more likely to die.
The post-exposure prophylaxis guidance was established after a review of the different options published yesterday in The Lancet Infectious Diseases. The report stems from an informal workshop on post-exposure prophylaxis, pulled together by the World Health Organization (WHO), that took place in Bethesda, Md., in June 2015.
The findings on Ebola signatures in blood samples were published today in Cell Host and Microbe by an international group of scientists from the University of Wisconsin at Madison, Pacific Northwest National Laboratory (PNNL), Ichan School of Medicine at Mount Sinai in New York City, the University of Tokyo, and Sierra Leone.
Weighing 6 leading countermeasures
West Africa's Ebola outbreak prompted intensive efforts to test several countermeasures that are in the development stages. The authors of the new report said post-exposure prophylaxis has an important role to play in outbreak settings, because it provides quicker protection than a vaccine and can add extra protection for health workers who are especially at risk.
Their review covers what's known about the strategies used and considered during the outbreak, and the guidance focuses on six leading countermeasures: the VSV-EBOV vaccine, as well as monoclonal antibodies (ZMapp and MIL77) and three small-molecule antivirals (favipiravir, GS-5734, and BXC4430).
The group sketched out a description of ideal Ebola post-exposure prophylaxis: an agent with proven efficacy, rapid onset with a window of protection, and broad activity against Ebola species and is well tolerated, easily administered, stable to transport and store, inexpensive, and readily available.
The group recommended scenarios, based on risk, that would warrant post-exposure prophylaxis. For example, skin-only contact while evaluating a patient with suspected Ebola infection poses an intermediate risk in which treatment could be considered. Treatment is recommended in the event of broken skin or mucous membrane contact with a patient's body fluids.
"One special circumstance that might warrant consideration of post-exposure prophylaxis is sexual contact and exposure to semen from male survivors of Ebola virus disease," the experts wrote.
The report includes a table weighing the pros and cons of the six leading post-exposure prophylaxis methods, along with suggested administration methods and dosing.
Vaccination and chemoprophylaxis could be used together to provide rapid and lasting protection, but the authors said more studies are needed to ensure that antiviral activity or monoclonal antibody activity doesn't interfere with the vaccine's immune response.
More research is needed to better define who should receive post-exposure prophylaxis and which drugs should be used, and studies should be designed now for use in future outbreaks, the experts said. They added that the impact of the strategy for preventing secondary cases should be modeled and studied further and that the supply pipeline and access should be enhanced so that people who need the treatments get them and furher studies can be done.
Distinguishing fatal from nonfatal Ebola
In the second study, researchers were able to conduct a detailed study of blood samples from Ebola patients because of a connection Yoshihiro Kawaoka, DVM, PhD, at the University of Wisconsin-Madison, made with a research fellow from Sierra Leone in the school's Department of Veterinary Medicine, according to a press release from the school. The fellow knew several well-positioned people in Sierra Leone's government.
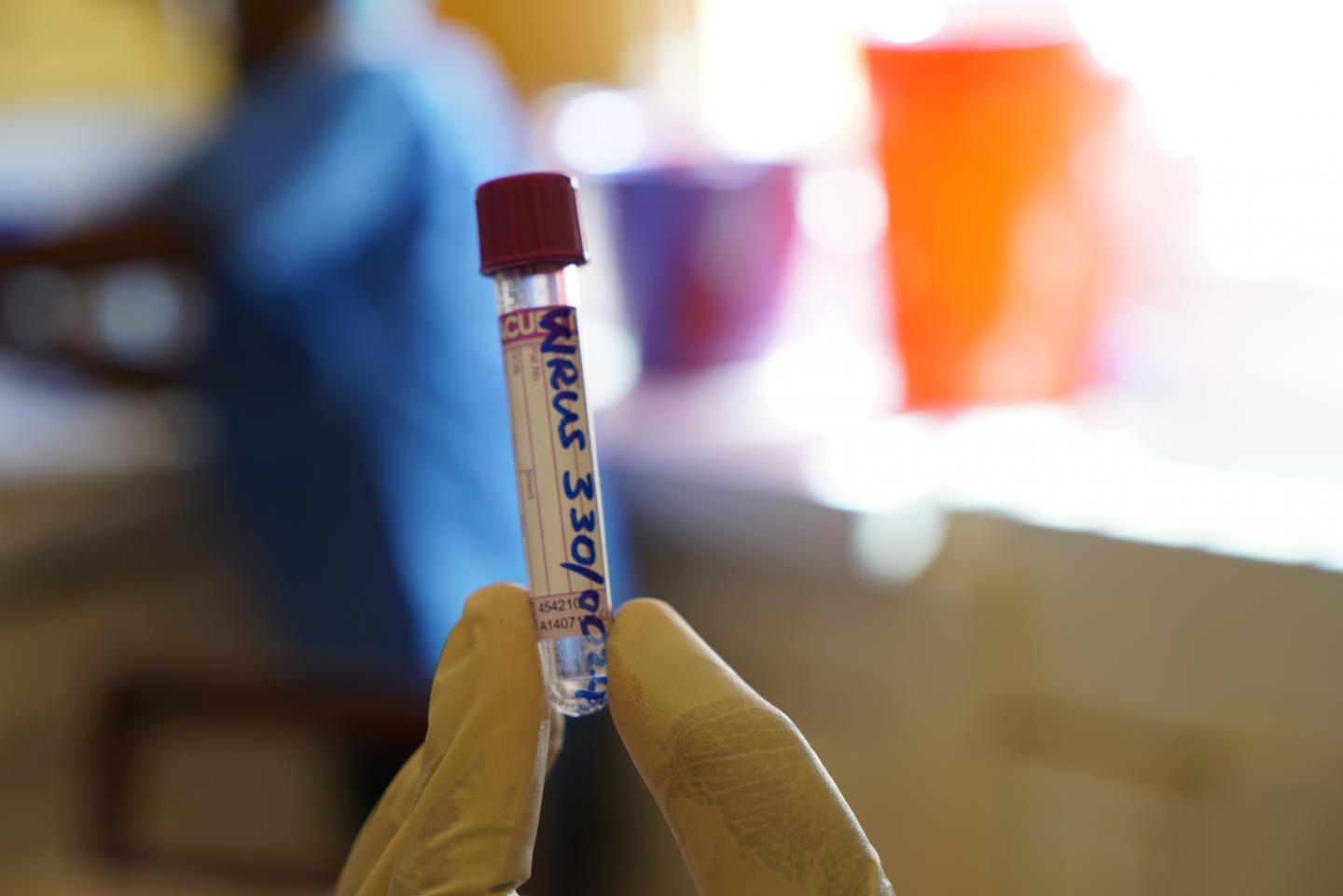
In December 2014 during the height of the outbreak, three of the researchers traveled to Sierra Leone and enlisted its government's support in securing lab space at a military hospital in Freetown to work on samples collected by authorized medical personnel.
With help from health workers and permission from patients, the group received 29 blood samples from 11 Ebola patients who survived and 9 from 9 patients who died. Kawaoka's team inactivated the virus before sending blood samples to University of Wisconsin and its partner labs for further study. For comparison, the team looked at blood samples from 10 healthy patients.
Katrina Waters, PhD, a biochemist at PNNL, said in the press release that scientists poured through thousands of molecular clues in each of the samples. "This may be the most thorough analysis yet of blood samples of patients infected with the Ebola virus," she said.
Survivors had different immune molecule profiles than those who died. In those who died, plasma cytokines were higher, metabolic responses were different, virus levels were higher, plasma lipids showed changes, and some types of immune cells were more activated.
Pancreatic enzymes leaked into the blood of those who died, hinting that they might play a role in tissue damage that's a hallmark in fatal cases.
In total, the investigators identified 11 markers that distinguished fatal infections from nonfatal ones. Lower levels of two of them stood out as more accurately predicting which patients would die: L-threonine, an amino acid, and vitamin D–binding protein.
The researchers said the findings might be useful for developing future treatments and may help clinicians prioritize scarce treatments and provide care to the sickest patients.
Trivalent vaccine in animals, health capacity gains
In other research, a study of trivalent vaccine against two Ebola virus strains and Marburg virus in nonhuman primates developed by Profectus BioSciences showed that a single dose protected all the animals from disease and death against lethal challenge 28 days after immunization, according to a study published yesterday in the Journal of Virology.
Researchers concluded that the trivalent vaccine (VesiculoVax) shows promise as a tool for battling filoviruses that are most commonly responsible for viral hemorrhagic fever outbreaks in sub-Saharan Africa. In October, Profectus announced that it had received a contract worth up to $22.5 million from the US National Institute of Allergy and Infectious Diseases to develop a version that also contains a component against Lassa virus.
Meanwhile, researchers from the US Centers for Disease Control and Prevention and their partners in West African countries affected by the Ebola outbreak described public health progress that was made during the outbreak in four key areas: emergency response, laboratory capacity, surveillance, and workforce development. They detailed their findings yesterday in Emerging Infectious Diseases.
The authors said though great strides have been made, achievements are fragile, especially given uncertain funding from donor countries.
See also:
Nov 15 Lancet Infect Dis abstract
Nov 16 Cell Host Microbe abstract
Nov 16 UW-Madison press release
Nov 15 J Virol abstract
Oct 3 CIDRAP News scan "Profectus awarded NIAID contract for vaccine against Ebola, related diseases"
Nov 15 Emerg Infect Dis report