Editor's note: This story was updated on Sep 21 with comments from lead author Aisling Vaughan, PhD, of Public Health England.
Because monkeypox was not immediately suspected in the most recent UK monkeypox case, healthcare workers (HCWs) were not wearing adequate personal protective equipment (PPE) for the disease and may have been exposed to the virus, UK officials reported today in Eurosurveillance.
They also noted that the patient—the second recently reported by Public Health England (PHE), on Sep 11—had two potential exposures. He had contact with a person who had a "monkeypox-like rash," and he also ate bush meat while visiting Nigeria. Nigeria has had 262 suspected and 113 confirmed monkeypox cases since September 2017.
The officials also provide more details on the first case, which PHE first reported on Sep 8. The cases appear unrelated, PHE has said.
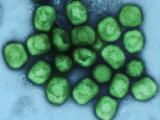
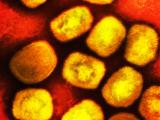
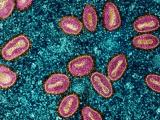
Monkeypox is an orthopoxvirus infection and is related to smallpox. The disease can also be confused with chickenpox, which is caused by an unrelated virus.
First case involves Nigerian officer
The first monkeypox case involves a male Nigerian naval officer who was attending a training course at a naval base in Cornwall in southwestern England. PHE was notified of his case on Sep 7.
The officer arrived in London from Abuja, Nigeria, on Sep 2, then took a train to the Cornwall base the same day. The next day, however, he sought primary care on the naval base after he spiked a fever and had swollen lymph nodes and a rash near his groin. Because the rash was suspected to be caused by a Staphylococcus infection, the man was prescribed antibiotics.
By Sep 6, though, the rash had spread to the man's torso, face and arms, and, after clinicians re-examined him they placed him in isolation in his quarters. Multiple samples, including swabs of the lesions, were sent to the PHE Rare and Imported Pathogen Laboratory (RIPL), whose scientists confirmed monkeypox by sequencing analysis.
The man is now in stable condition and is improving, according to the report.
Multiple exposures in 2nd case
The second patient is a UK man of unknown age who returned to the country from a 22-day vacation in Nigeria on Sep 4 via a flight from Paris. He sought care at the Accident and Emergency Department at Blackpool Teaching Hospitals on the northwest coast on Sep 6 for fever, swollen lymph nodes, a scrotal lump, and an itchy maculopapular rash, which is a flat, typically red area covered with small, connected bumps.
The man said the rash first appeared in Nigeria before his trip back to England and affected his face before spreading to other areas, including the palms of his hands, and had become pustular. He has also had a different febrile illness a week before coming to the Blackpool hospital and had received antibiotics for that, the authors of the report said.
On examination at the hospital, the man had "crops of vesicles that were progressing and lesions on the mucosal surfaces of the mouth," the report said. He was isolated at the hospital, and the RIPL confirmed monkeypox DNA by multiple molecular tests.
"Although the patient was isolated," the report said, "monkeypox was not initially suspected because the first lesions appeared in the groin, and the wearing of full personal protective equipment (a filtering face-piece with three indicating levels of protection [FFP3], eye protection, gloves, and sterile disposable gown) was not implemented immediately."
A "number" of HCWs were potentially exposed because of the PPE lapse, the authors wrote. The man was transferred to a specialized unit at the Royal Liverpool University Hospital on Sep 10 and remains in stable condition.
Although the ultimate source of the man's infection is unknown, he reported contact with a person who had a monkeypox-like rash at a large family gathering and ate bush meat during a visit to a rural area in southern Nigeria.
Risk to exposed HCWs deemed low
Lead author Aisling Vaughan, PhD, an epidemiologist with the PHE's National Infection Service, said of the HCWs who attended to the man without wearing optimal PPE, "The risk is deemed to be low."
She told CIDRAP News, "It is not that the healthcare workers were exposed because of improper PPE. Before monkeypox was considered as a possibility, the PPE they wore was not deemed sufficient for the management of monkeypox—for example, they wore surgical masks instead of respirators. Once monkeypox was suspected, appropriate PPE was worn straightaway.
"Therefore, some HCW workers caring for or exposed to the patient prior to the diagnosis may have been exposed."
Vaughan added, "It is advised that HCWs apply contact and droplet precautions by wearing a filtering face-piece with three indicating levels of protection (FFP3 in Europe), eye protection, gloves, and sterile disposable gown. The US equivalent is the N95, although the FFP3 offers higher protection."
She said none of the potentially exposed HCWs are showing symptoms. Contacts of the patient, including HCWs, are under active or passive surveillance, depending on their level of contact or exposure risk.
When asked how many HCWs were exposed, she said, "We are not disclosing a breakdown of the figures at present."
Public health response
The investigators write in the report, "Although there was no evidence for an epidemiological link between the two cases in the UK, both had travelled in southern Nigeria before coming to the UK. While it was difficult to obtain clear travel histories from the patients, both cases had visited areas in southern Nigeria (Lagos State, Federal Capital Territory, Rivers State and Delta State), where cases of monkeypox have recently been reported."
The Nigeria Centre for Disease Control is conducting epidemiologic investigations to identify contacts of the two cases and to determine the source of infection, the authors noted.
In the UK, PHE is following up on 229 of 243 contacts; 93 of them are under active surveillance, while 136 are under passive surveillance. Vaughan confirmed that some of the 93 under active surveillance are HCWs. Officials are also seeking out the other 14 as-yet-unreached contacts.
The report says that 27 HCWs at the referral hospitals for both patients (Royal Free and Royal Liverpool) were offered the smallpox vaccine before being exposed to the patients.
In France, officials have contacted passengers who took the same flight from Lagos to Paris with the second case-patient.
The officials conclude the report, "The diagnosis of two unconnected monkeypox cases within a short time frame in the UK is a highly unusual occurrence and most probably reflects the ongoing monkeypox transmission events in a number of African countries, including Nigeria.
"This incident reinforces the importance of infectious disease surveillance, clinical awareness, and early recognition and isolation, as well as the need to obtain a full travel history for all patients. This incident also highlights the importance of global health security initiatives and the rapid sharing of information."
See also:
Sep 20 Eurosurveill report
Sep 11 CIDRAP News scan on second case
Sep 12 CIDRAP News scan on Nigeria outbreak