A new antibiotic to treat gonorrhea has shown promising results in a small phase 2 trial.
The results of the trial, published yesterday in The New England Journal of Medicine, show that zoliflodacin, a single-dose oral antibiotic with a mechanism of action that differs from currently available therapies, was highly effective in treating patients with urogenital and rectal gonorrhea infections and was well-tolerated. But the cure rates were lower in patients who had gonorrhea infections of the throat (pharyngeal).
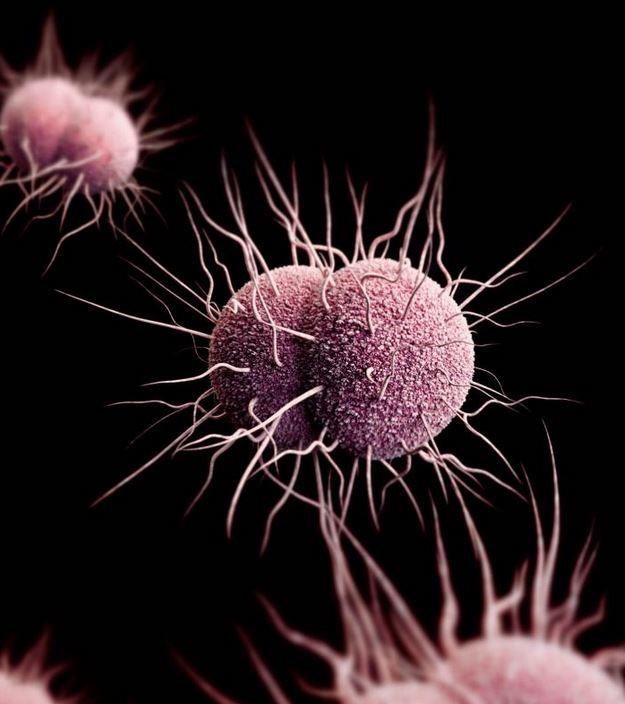
Zoliflodacin is one of three antibiotics in development for Neisseria gonorrhoeae, one of the most common sexually transmitted infections. Developed by Entasis Therapeutics, the drug has been "fast-tracked" for development by the US Food and Drug Administration and will soon be tested in a larger, multinational phase 3 trial conducted in partnership with the Global Antibiotic Research and Development Partnership (GARDP).
The need for new treatment options for gonorrhea has grown urgent as resistance to the current treatment regimen of azithromycin and ceftriaxone rises worldwide. Although this regimen remains mostly effective, it is the last remaining treatment option for N gonorrhoeae, a bacterium that develops resistance quickly and has cycled through several other antibiotics. The World Health Organization (WHO) has warned that widespread gonorrhea treatment failure could be on the horizon if new drugs aren't developed.
"The results are very encouraging, because we have not had a new drug come down the pipeline in a long time for gonorrhea, and this is the perfect time, now that we are starting to see resistance," lead investigator Stephanie Taylor, MD, a professor of medicine and microbiology at Louisiana State University School of Medicine, told CIDRAP News.
High cure rates for urogenital, rectal infections
The trial, which was sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), enrolled 179 patients (167 men and 12 women) who were recruited from sexual health clinics in Louisiana, Washington, Indiana, Alabama, and North Carolina from November 2014 through December 2015. Individuals were eligible to participate if they had signs and symptoms of urogenital gonorrhea, untreated urogenital gonorrhea, or sexual contact in the preceding 14 days with a person who had gonorrhea.
Thirty-eight participants with negative gonococcal cultures were excluded from the efficacy analysis, leaving 141 patients in the microbiologic intention-to-treat (micro-ITT) population. These patients were randomly assigned to receive a single dose of oral zoliflodacin (either 2 or 3 grams [g]) or a single 500 milligram intramuscular shot of ceftriaxone.
The primary efficacy outcome was the proportion of urogenital microbiologic cure in the micro-ITT population. Secondary efficacy outcomes included the proportion of rectal or pharyngeal microbiologic cure. The primary safety outcome was the proportion of adverse events.
In the 141 patients evaluated 6 days after treatment, urogenital infections were cured in 55 of 57 participants (96%) who received 2 g of zoliflodacin, 54 of 56 participants (96%) who received 3 g of zoliflodacin, and 28 of 28 of participants (100%) who received the shot of ceftriaxone. Rectal infections were cured in all 5 participants who received 2 g of zoliflodacin, all 7 who received 3 g of zoliflodacin, and all 3 treated with ceftriaxone. But among the participants with pharyngeal gonorrhea, only 4 of 8 (50%) who received 2 g of zoliflodacin and 9 of 11 (82%) who received 3 g were cured, compared with 4 of 4 patients (100%) who received ceftriaxone.
A total of 84 adverse events were reported, with 24 and 37 reported in those who received 2 g or 3 g of zoliflodacin, respectively, and 23 in the ceftriaxone group. Investigators determined that 21 of the adverse events were related to zoliflodacin, and most were gastrointestinal and self-limiting. Post-treatment testing of gonorrhea isolates showed no resistance to zoliflodacin.
Taylor and her coauthors note that while the cure rate of zoliflodacin for urogenital and rectal gonorrhea met the criterion for efficacy (95% or higher) in treating uncomplicated gonorrhea, it failed to meet it for pharyngeal infections, which are known to be more difficult to treat. Taylor said this was not entirely surprising, since other oral antibiotics have been less effective against gonorrhea infections in the throat. She suggested the lower efficacy could be caused by poor drug penetration into pharyngeal tissue, rather than resistance to zoliflodacin.
"We're hoping to be able to overcome this at some point, because it is an important site, and we want to be able to eradicate the organism at all sites," Taylor said. "This will be something we'll be working on, and a higher dosage could potentially help."
Taylor and her colleagues also note that the study was limited by low enrollment of women and the low number of participants with rectal gonorrhea.
Crucial next steps
Nonetheless, the results pave the way for the phase 3 trial, which will be conducted in the Netherlands, South Africa, Thailand, and the United States starting next year. Results from that trial will determine whether zoliflodacin will be approved by the FDA and become an alternative option for treating gonorrhea.
If the results are positive and zoliflodacin is ultimately approved for gonorrhea infections, Taylor said she could envision the drug becoming the recommended treatment because it's easier to administer, with ceftriaxone as a fall-back option.
"We want to have an oral agent rather than an injectable agent, and we also want to stockpile or save ceftriaxone," she explained. Zoliflodacin could also replace azithromycin in the dual treatment regimen, which was adopted to slow the development of resistance to ceftriaxone.
Alan Katz, MD, MPH, an STD expert and public health professor at the University of Hawaii who was not involved in the study, said that while having an oral option to treat gonorrhea would be great, he does have concerns about the lower efficacy in pharyngeal gonorrhea, especially since pharyngeal infections are common in gay men and have also been reported in heterosexual men.
"As oral sex is a common practice, we would benefit greatly from developing additional therapeutic options that will address gonococcal infections at both urogenital and pharyngeal sites," Katz told CIDRAP News.
The WHO estimates that there are more than 78 million new cases of gonorrhea each year, and the Centers Disease Control and Prevention recently reported a 67% increase in US gonorrhea infections from 2013 through 2017. If gonorrhea goes untreated or if treatment fails, it can lead to pelvic inflammatory disease, ectopic pregnancy, infertility, and increased risk of HIV infection.
See also:
Nov 7 N Engl J Med abstract
Nov 7 N Engl J Med commentary