Data from a multi-country randomized clinical trial published yesterday in the New England Journal of Medicine provide evidence that a shorter drug regimen works just as well in certain patients with multidrug-resistant tuberculosis (MDR-TB) as the longer regimen.
The results of the first stage of the phase 3 STREAM (Standard Treatment Regimen of Anti-Tuberculosis Drugs for Patients with MDR-TB) trial showed that in patients with rifampin-resistant TB that was susceptible to fluoroquinolones and aminoglycosides, a treatment regimen of 9 to 11 months was noninferior to the standard 20-month regimen, producing a favorable outcome in 79% of participants while the longer treatment was effective in 80% of patients.
The findings support previous studies of the "Bangladesh regimen," a 9- to 11-month treatment that produced cure rates above 80% in patients in Bangladesh but had not been tested against the longer regimen.
The results of the trial mean that, for some MDR-TB patients, treatment could be significantly shorter and cheaper, which could make it more likely that they follow it through to completion. The length and costs of the standard MDR-TB treatment, along with the side effects associated with some of the second-line antibiotics, are among the reasons that treatment success rate for MDR-TB is only 54%.
"We know from programmatic data that the 20-24-month regimen has a number of major drawbacks, including the difficulty of completing such a long treatment, the significant side-effects of the drugs used and poor treatment outcomes," study co-leader Andrew Nunn, MSc, a senior scientist and professor of epidemiology at University College London, said in a university news release. "Shorter, more effective and safer regimens are urgently needed."
Similar efficacy, safety outcomes
The shorter regimen tested in the STREAM trial consisted of high-dose moxifloxacin, clofazimine, ethambutol, and pyrazinamide over 40 weeks, supplemented by kanamycin, isoniazid, and prothionamide during the first 16 weeks of treatment. This slightly modified version of the Bangladesh regimen was compared with the 20-month MDR-TB regimen recommended in the World Health Organization's (WHO's) 2011 guidelines.
From July 2012 through June 2015, investigators enrolled and screened 689 participants from Ethiopia, Mongolia, South Africa, and Vietnam. Of these patients, 424 underwent randomization on a 2:1 basis, with 282 assigned to the short regimen and 142 to the long regimen. The modified intention-to-treat group included 389 patients, of whom 369 were included in the modified intention-to-treat efficacy analysis.
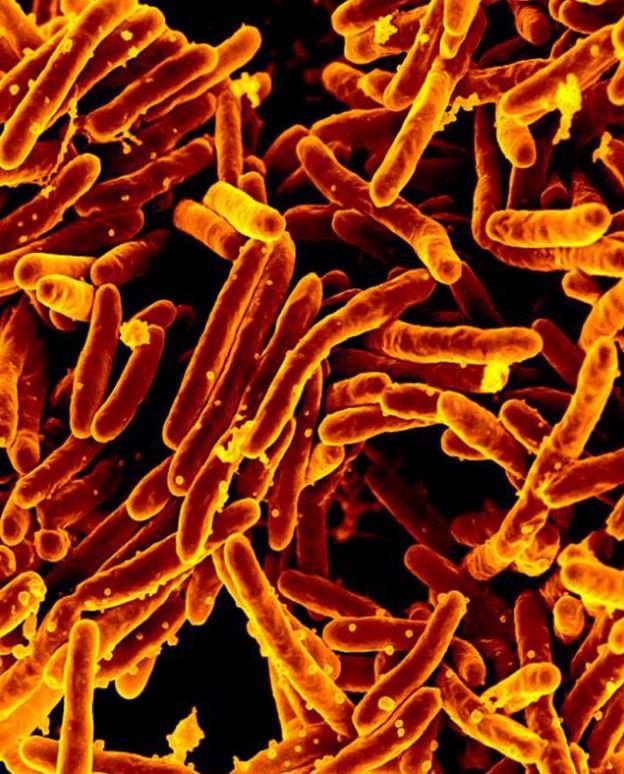
The primary efficacy outcome of the trial was a culture that was negative for Mycobacterium tuberculosis at 132 weeks after randomization, and the primary safety outcome was the occurrence of severe adverse events at any time during treatment. The noninferiority margin was 10 percentage points.
The results showed that favorable status was attained by 78.8% of patients (193 of 245) in the short-regimen group and 79.8% of patients (99 of 124) in the long-regimen group. With adjustment for HIV status, the difference was 1 percentage point (95% confidence interval [CI], –7.5 to 9.5, P = 0.02).
The noninferiority results were consistent in the per-protocol population, with 81.9% of patients (186 of 227) in the short-regimen group achieving favorable status compared with 80.7% of patients (63 of 87) in the long-regimen group (adjusted difference, –0.7 percentage points; 95% CI, –10.5 to 9.1, P = 0.02).
The comparison of safety outcomes found that an adverse event of grade 3 or higher occurred in 48.2% of patients (136 of 282) treated with the short regimen and 45.4% of patients (64 of 141) on the long regimen. In addition, electrocardiogram readings showed that more patients in the short-regimen arm experienced prolongation of the QT interval (11% vs. 6.4% in the long-regimen arm), a syndrome that causes irregular heart rhythms. As a result, some of those patients received medication adjustments.
There were also more deaths among short-regimen patients, more liver and ear disorders, and more acquired resistance to fluoroquinolones and aminoglycosides compared with patients on the long regimen, although the differences were not considered statistically significant.
Shorter, simpler regimens needed
The results are meaningful, because shorter regimens could help improve the poor success rate for MDR-TB treatment, which is significantly lower than the 82% success rate for patients with susceptible TB and is hindering global efforts to tackle the disease.
While overall TB incidence has fallen in recent years, the incidence of drug-resistant MDR-TB, which was diagnosed in 558,000 people and caused 230,000 deaths in 2017, has risen.
In response, the WHO has sought to include shorter treatments in its guidelines for MDR-TB treatment. In 2016, the WHO used the data from the Bangladesh studies to recommend the shorter regimen for certain MDR-TB patients—those who haven’t previously been treated with second-line drugs and whose disease remains susceptible to fluoroquinolones and aminoglycosides. When those guidelines were updated in December 2018, preliminary data from the STREAM trial was included to justify that recommendation.
Mel Spigelman, MD, president and CEO of the TB Alliance, told CIDRAP News that the study is an important step in efforts to improve treatment for MDR-TB patients.
"TB Alliance applauds rigorous scientific studies that answer important questions about treating drug-resistant TB," Spigelmen said. "Resources to support [research and development] are needed to further build out the evidence base and provide the data required to introduce improved treatments that are shorter, effective, and affordable."
Despite the encouraging results, the STREAM trial investigators and other experts agree that more research on shorter, simpler MDR-TB drug regimens is needed. A simpler regimen would ideally include only oral medications. Gavin Churchyard, MD, PhD, a TB expert at the Aurum Institute in South Africa, notes in an accompanying commentary that the short regimen used in the trial still calls for 4 months of painful injections with kanamycin, an aminoglycoside that's been linked to hearing loss and kidney problems in MDR-TB patients.
"Thus, although the shorter regimen is definitely better when it comes to treating multidrug-resistant and rifampin-resistant tuberculosis, it is not good enough," Churchyard writes.
A second stage of the STREAM trial is currently evaluating whether a fully oral version of the short regimen—which would avoid the toxic effects associated with kanamycin—is as effective as the longer regimen.
See also:
Mar 13 N Engl J Med abstract
Mar 13 N Engl J Med editorial
Mar 13 University College London news release