A team of US and British scientists are reporting the successful treatment of a life-threatening mycobacterial infection using genetically engineered bacteriophages.
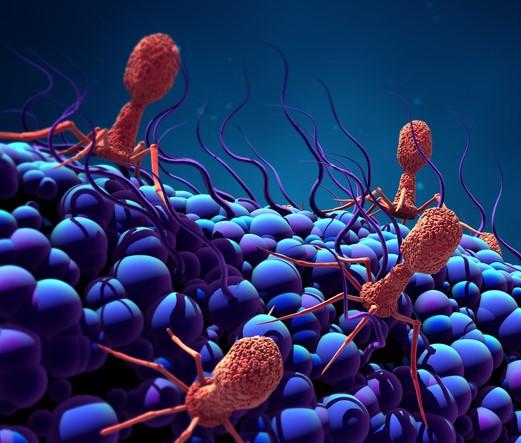
In a case report published yesterday in Nature Medicine, the team describes the efforts to save a young cystic fibrosis patient in England struggling with a multidrug-resistant (MDR) Mycobacterium abscessus infection following a double lung transplant. It's the latest in a handful of cases in which bacteriophages, the ubiquitous viruses that attack and destroy bacteria, have been used as a last-resort treatment for patients with MDR bacterial infections. But it's the first using genetically engineered phages.
Over a 7-month period, a cocktail of three bacteriophages was isolated and developed by scientists at the University of Pittsburgh from a library of more than 15,000 phages. And 6 months after the patient began receiving the cocktail, the infection has largely cleared.
"We're in uncharted territory, but the patient has done incredibly well, and I think we're through the most serious part of the infection," study co-author Graham Hatfull, PhD, a professor of biological sciences at the University of Pittsburgh, told CIDRAP News.
A search for phages begins
Although the September 2017 lung transplant at London's Great Ormond Street Hospital went well for 15-year-old Isabelle Carnell-Holdaway, the pre-existing infection with non-tuberculosis mycobacteria—which had been treated with antibiotics for 8 years—began causing problems soon after the surgery.
The antibiotics had stopped working, and because she was taking immunosuppressive drugs to prevent rejection of the new lungs, her body was unable to fight the bacteria. The infection spread from the surgical incision to the liver and throughout the body, popping up in skin lesions on her arms and legs. No treatment options remained.
That's when James Soothill, MD, a microbiologist at the hospital, got in touch with Hatfull. The two had previously met at a conference on phage therapy, and Soothill, knowing of Hatfull's work with bacteriophages, sent him an email describing the patient. There was also another cystic fibrosis patient at the hospital experiencing the same difficulties.
"He said that they have these patients that have this particular profile, and he was curious—and I was curious—as to whether we might have phages that would infect them," Hatfull said. "I'm not sure that either of us thought it was going to end up a therapy, but we were interested in it from a basic research question."
Hatfull had a lot of phages to choose from. He leads the Howard Hughes Medical Institute's SEA-PHAGES (Science Education Alliance Phage Hunters Advancing Genomics and Evolutionary Science) programs, which gives college students at more than 150 institutions around the world the opportunity to collect and perform genome sequencing on bacteriophages, which can be found in all sorts of environments, from soil to sewage to seawater. Hatfull has spent more three decades building this phage repository.
Of the 15,000 bacteriophages in the collection, more than 10,000 target Mycobacterium smegmatis. And with the genomic data on 1,800 of these phages, Hatfull knew that a subset would attack other types of mycobacteria, including M abscessus. But because phages need to match the particular strain of bacterium there was more work to be done.
"Different strains of Mycobacterium abscessus have different susceptibility to the different phages…so we needed the phages that would be specific to that particular strain in that particular patient," he said.
Once he received samples of the bacterial strains from the two patients, Hatfull and his team began their search. One of the patients died before they could find the right match. But they ultimately isolated three phages—named Muddy, ZoeJ, and BPs—with potential against Carnell-Holdaway's strain (M abscessus subspecies massiliense). Muddy, discovered by a student in South Africa, efficiently killed the strain. But ZoeJ and BPs needed some genetic tweaking to make them more efficient killers.
"If we wanted to use more than one phage, we needed to do something to convert some of the miserable-looking guys into something that would work efficiently, and we have engineering tools and strategies we can use to do genetic manipulation," Hatfull explained. "We deployed those tools to get two more phages and get a cocktail of three."
After Hatfull and his colleagues in Pittsburgh completed the lengthy process of growing and amplifying the phages, then purifying and testing them to make sure there were no toxins and that the cocktail would be safe for intravenous (IV) use, the team of clinicians in London, led by Helen Spencer, MD, tried a topical test dose of the cocktail on Carnell-Holdaway's incision in June 2018. IV therapy began the next day. She responded well, with no signs of adverse effects, and was sent home after 9 days. IV and topical treatment continued at home.
After 6 weeks, the liver infection had cleared, and the surgical wound and lesions slowly disappeared over the following months. Only one or two of the lesions remain. Although the authors of the study cannot definitively say these improvements would have occurred without the phage therapy, they note that patients with similar conditions typically have high morbidity and mortality.
The future of phage therapy
Steffanie Strathdee, PhD, co-director of the Center for Innovative Phage Applications and Therapeutics (IPATH) at the UC San Diego School of Medicine, says the case is exciting on a number of levels. "It's the first use of genetically modified phages in a human being that was successful, and it's the first Mycobacterium infection in a human that's been treated with phages, and that means there's promise that we could use phage therapy to treat tuberculosis at some point," she said.
For Strathdee, there's also a personal connection. Her husband, Tom Patterson, PhD, was successfully treated in 2016 with a bacteriophage cocktail for an MDR Acinetobacter baumannii infection that had left him fighting for his life, and they've co-authored a book on the experience—The Perfect Predator. Patterson's doctor and IPATH co-director Robert Schooley, MD, advised on Carnell-Holdaway's case, and Strathdee was involved from the very beginning, communicating with Carnell-Holdaway's mother throughout the treatment process.
"I'm just really happy that my husband and I could be part of it in a small way, because there's nothing better than knowing that the pain and agony that you and your family went through is paying off and saving other lives" she said.
The question is what the future holds for phage therapy, which to date has been used only in individual cases. The specificity of phages, Hatfull says, is a double-edged sword. On the one hand, because phages act as "guided missiles" and attack only a particular bacterial strain, they don't have some of the side effects of broad-spectrum antibiotics, which can foster the emergence of multidrug resistance and wipe out beneficial bacteria in the gut. The toxicity is also low, because phages aren't chemicals and don't target human cells.
"The specificity is definitely our friend in terms of using phages in antimicrobial treatment," Hatfull said.
But specificity is also a problem, because phages that work for one strain of bacteria don't necessarily work on other strains. Muddy, ZoeJ, and BPs, for example, don't efficiently kill other M abscessus clinical isolates. "That's really at the root of the problem of [not] having a broader and more generalizable therapy," he said.
But Strathdee says that, with the ability to genetically engineer phages, there's the possibility that scientists can create phages that target more than one strain of a bacterial species. "If you could edit the genes to just be a little broader spectrum, that would be great," she said. "We have a lot to learn still, but I think there's great potential."
See also:
May 8 Nature Med study
Nov 16, 2017, CIDRAP News story "To save a life, doctors turn to bacteria-killing viruses"