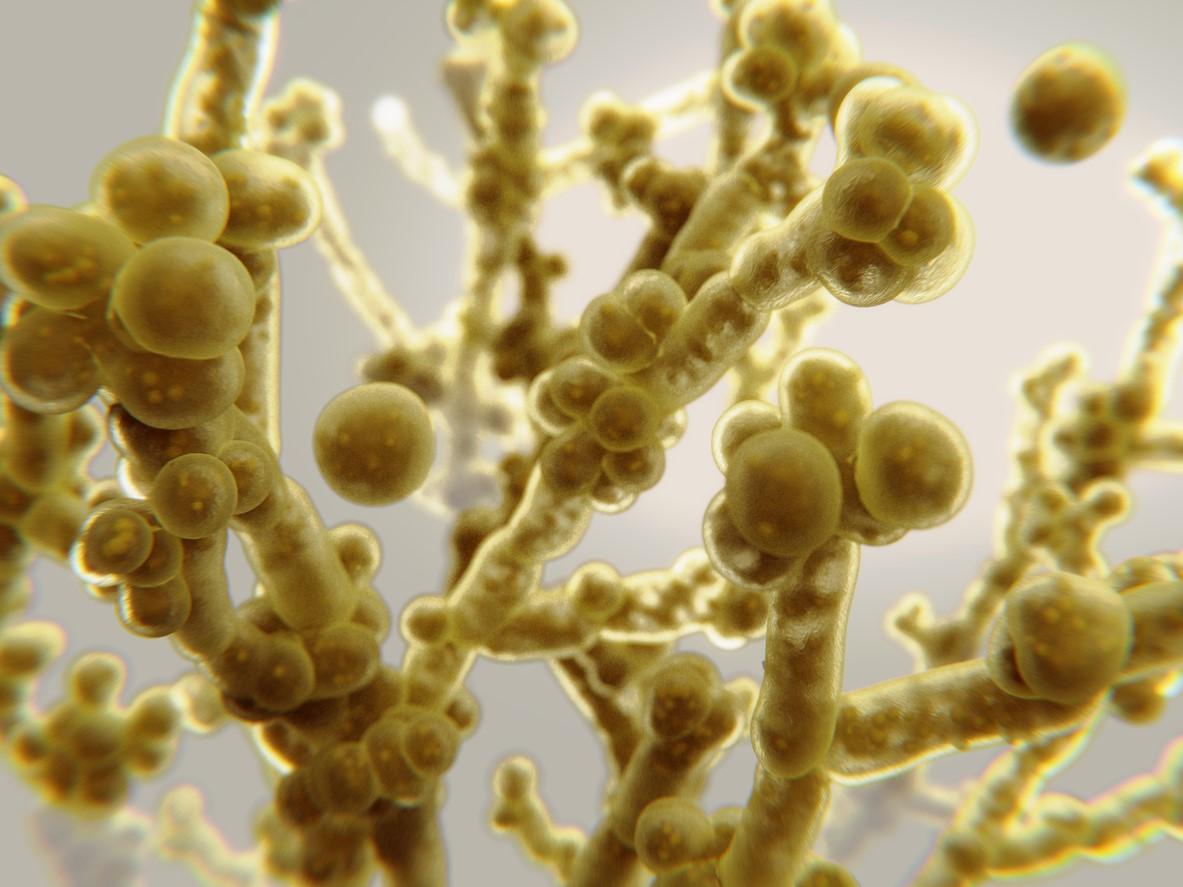
Two studies presented last week at the annual conference of the American Society for Microbiology (ASM) highlight the rising prevalence of the multidrug-resistant fungal pathogen Candida auris in US hospitals and the need for better antifungal susceptibility testing.
Substantial increase since 2022
In the first study, researchers with French diagnostics company bioMerieux reported that a retrospective analysis of blood cultures collected in US hospitals from 2020 to March 2023 found a significant increase in C auris bloodstream infections over the past year.
Using bioMerieux's proprietary blood culture identification panel and a cloud-based network that provides near real-time surveillance, the researchers found that the average detection rate for C auris in bloodstream infections rose from 0.014% before October 2022 (July 2020 to September 2022) to 0.057% after October 2022 (October 2022 to March 2023). Beginning in October 2022, C auris detection rates rose in the Midwest, South, and Northeast Census regions, with the highest detection rate observed in the Northeast and the largest increase seen in the South.
The findings add to recent data released by the Centers for Disease Control and Prevention (CDC) showing that C auris infections in US hospitals rose by 59% in 2020 and 95% in 2021. The pathogen was identified in Japan in 2009 and first detected in the United States in 2016.
The study results confirm that we must continue to emphasize public health interventions under the leadership of the Centers for Disease Control and Prevention in order to meet the continuing challenge posed by antimicrobial-resistant C. auris and protect community health.
The increase in C auris infections in US hospitals over the last few years has been partly attributed to the COVID-19 pandemic. In many hospitals around the country, staff responsible for maintaining the infection prevention and control strategies that can reduce the incidence of pathogens like C auris, which spreads easily in healthcare settings and is difficult to eradicate, were diverted to COVID care. In addition, severely ill COVID-19 patients were increasingly susceptible to C auris and other healthcare-associated infections.
Another recent CDC study found that the overall in-hospital mortality rate for C auris infections was 34%, and 47% for bloodstream infections.
"The study results confirm that we must continue to emphasize public health interventions under the leadership of the Centers for Disease Control and Prevention in order to meet the continuing challenge posed by antimicrobial-resistant C. auris and protect community health," presenting author Tristan T. Timbrook, PharmD, MPH, bioMerieux's director of Health Economics Outcomes Research, Global Medical Affairs, said in an ASM press release.
Better susceptibility testing needed
One of the reasons why C auris infections are so deadly is that the yeast has shown resistance to all classes of antifungals used to treat invasive Candida infections. That makes antifungal susceptibility testing (AFST) critical for guiding effective treatment. But there are no C auris-specific AFSTs currently available at US hospitals, so clinicians have to send C auris isolates out for susceptibility testing.
To evaluate how the AFST platforms currently used by specialty or public health laboratories for a variety of invasive fungal pathogens perform for C auris, researchers with Indiana University conducted susceptibility testing on 50 C auris isolates collected from the CDC's Antibiotic Resistance Laboratory Network and Indiana University Health Hospital. They then compared the results to a reference method.
The results showed that two of the tests were in 100% agreement for susceptibility to echinocandins, one the antifungals used to treat C auris infections. But those same tests performed poorly with fluconazole and amphotericin B. Other tests incorrectly reported resistance to an antifungal when a C auris strain was susceptible or showed susceptibility when a strain was resistant, according to an ASM press release.
The researchers say the findings highlight the need for a Food and Drug Administration-approved AFST for C auris.