Pennsylvania-based Venatorx Pharmaceuticals announced yesterday that it has received a $167 million contract from the Biomedical Advanced Research and Development Authority (BARDA) to develop a novel oral antibiotic for complicated urinary tract infections (cUTIs).
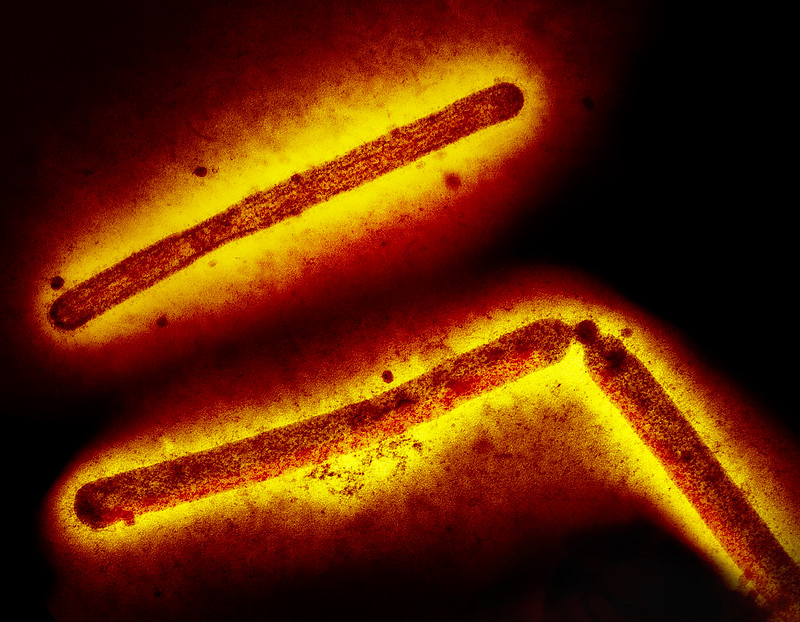
The BARDA award will support development of ceftibuten-ledaborbactam etzadroxil, which combines a cephalosporin antibiotic with a novel, broad-spectrum boronic acid beta-lactamase inhibitor. Venatorx says the combination may offer a new oral treatment option for outpatient therapy to treat cUTIs and other serious bacterial infections caused by multidrug-resistant Enterobacterales.
An estimated 2.8 million cUTI cases are diagnosed annually in the United States, and cUTIs caused by drug-resistant bacteria are on the rise.
"Currently, there are no approved oral antibiotics that are effective in the treatment of drug-resistant gram-negative bacterial infections to help address increasing drug-resistant bacterial infections globally," Venatorx President and CEO Christopher Burns, PhD, said in a company press release. "We believe that oral ceftibuten-ledaborbactam etzadroxil could play an important role in treating drug-resistant gram-negative infections, preventing unnecessary hospitalizations, and saving lives."
Ceftibuten-ledaborbactam etzadroxil has been granted Qualified Infectious Disease Product and Fast Track designation by the US Food and Drug Administration (FDA) and has recently completed phase 1 clinical studies. The drug will advance directly to phase 3 trials under the BARDA contract.
NDA approved for ceftobiprole
In other antibiotic-development news, Swiss biopharmaceutical company Basilea Pharmaceutica announced last week that the FDA has approved its New Drug Application (NDA) for ceftobiprole. The company is seeking approval for treating patients with Staphylococcus aureus bacteremia (SAB), acute bacterial skin and skin structure infections, and community acquired bacterial pneumonia.
"We are pleased with the FDA's acceptance of our New Drug Application, which is another important step towards bringing ceftobiprole to patients with severe bacterial infections in the US, as there is a high medical need for new antibiotic treatment options, especially in complicated SAB," Basilea Chief Medical Officer Marc Engelhardt, MD, said in a press release.