A new forecasting study by Chinese researchers suggests the long-term impacts of climate change could include higher global antimicrobial resistance (AMR) levels.
In a study published today in Nature Medicine, the researchers projected that if countries continue to pursue fossil fuel-intensive development strategies that push up global temperatures, global AMR prevalence could rise by more than 2% globally by 2050, with poorer nations bearing more of the burden than wealthier nations.
But the model created by the researchers also projected that if the low-resource countries where AMR is already a significant problem worked to meet sustainable development goals, they could cut global AMR levels by more than 5% by 2050—more than twice the impact estimated from cutting human antibiotic use in half.
The researchers say the findings highlight the need for a multifaceted and collaborative approach to effectively managing AMR, particularly in countries that are already facing substantial AMR burdens and have limited resources.
The role of climate, socioeconomic factors
To create their model, a team led by researchers from Peking University analyzed 4,502 AMR surveillance records involving 32 million tested bacterial isolates collected from 101 countries from 1999 through 2022.
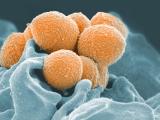
The datasets, obtained from the Global Antimicrobial Resistance and Use Surveillance System and other regional AMR surveillance networks, focused on six high priority drug-resistant pathogens—third-generation cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae, and carbapenem-resistant E coli, K pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa.
The primary aim of the study was to investigate the potential climate and socioeconomic determinants of AMR, particularly in low- and middle-income countries (LMICs), which have been disproportionately affected by both AMR and climate change.
"LMICs face unique challenges in the fight against AMR due to issues such as poverty, corruption, inadequate sanitation and poor testing infrastructure, which exacerbate AMR compared with their high-income country (HIC) counterparts," the study authors wrote. "Developing effective AMR intervention strategies within the resource and infrastructure constraints of LMICs is crucial."
The data showed higher average AMR prevalence in regions such as South Asia, the Middle East and North Africa, and sub-Saharan Africa. In a multivariable analysis, the researchers found that average AMR prevalence was positively correlated with air pollutant fine particulate matter and surface runoff—environmental factors that have previously been identified as influencing AMR—as well as temperature change, which was significantly associated with higher prevalence of carbapenem-resistant A baumannii.
Higher AMR prevalence was also positively correlated with higher out-of-pocket healthcare costs and antibiotic consumption (AMC). In contrast, average AMR prevalence was negatively correlated with subsurface runoff, higher government spending on health, and greater immunization coverage.
Developing effective AMR intervention strategies within the resource and infrastructure constraints of LMICs is crucial.
To explore the role these factors may play in future outcomes, the researchers then developed different scenarios based on varying levels of socioeconomic development, AMC, and greenhouse gas concentration trajectories. Sustainable development efforts included four specific government interventions: increased health investment, reduced out-of-pocket healthcare expenses, improved access to water, sanitation, and hygiene (WASH) services, and expanded immunization coverage.
The results showed that, if countries pursue a fossil-fuel–intensive development pathway with the highest greenhouse gas concentration trajectory—a path that could lead to a temperature increase of 4 to 5 degrees Celsius by the end of the century—global AMR levels will rise by 2.4% globally compared with a sustainable low-emission pathway. Broken down by income level, the projected increases were 0.9% in high-income countries, 1.5% in upper-middle-income countries, 4.1% in LMICs, and 3.3% in low-income countries.
Under a scenario in which countries reduce AMC by 50%, global AMR levels would be reduced by 2.1%. But if countries were to pursue sustainable development goals, AMR levels could be reduced by 5.1%. The measure associated with the greatest reduction in AMR levels (3.6%) was reducing out-of-pocket healthcare expenses.
Climate change could still exacerbate the problem
Although antibiotic use is the key driver in the development and spread of drug-resistant pathogens, the researchers say the different scenarios they simulated underscore the impacts of socioeconomic factors on AMR and the limits of focusing on reduced antibiotic use as a standalone strategy.
"Specifically, compared with limiting AMC, sustainable development efforts that emphasize universal access to WASH services, comprehensive immunization coverage, adequate health investments and affordable out-of-pocket healthcare costs can help LMICs better address AMR challenges," they wrote.
They add that the findings support the blueprint laid out in the 2024 United Nations General Assembly political declaration on AMR. Among the series of recommendations that aim to reduce global AMR deaths by 10% by 2030, the document called for all countries to have basic WASH services in all healthcare facilities by 2030. It also called for countries to promote routine immunization, invest in resilient and sustainable health systems, and accelerate efforts to ensure access to essential health services.
But even if countries do achieve some of these sustainable development goals, the authors say climate change could still raise AMR levels, even if a causal link has not yet been established and the exact mechanism is unclear. It could spread AMR through more extreme weather events that bring heavy rain and flooding, or by altering animal habitats and natural microbial ecosystems in ways that increase the spillover of zoonotic and vector-borne diseases.
"These challenges highlight the urgent need for global cooperation in developing and implementing strategies to address the interconnected and evolving threats posed by climate change and AMR," they wrote.