Sometime next year, the Centers for Disease Control and Prevention (CDC) will publish guidelines for one of the first new sexually transmitted infection (STI) prevention tools in decades.
The tool—the tetracycline antibiotic doxycycline—is not new. In fact, it was first approved by the Food and Drug Administration in 1967 and has since then been used to treat a variety of bacterial infections, from respiratory infections to skin infections and STIs like chlamydia and syphilis. Safe, inexpensive, and widely available, it's the most commonly used tetracycline and is on the World Health Organization's list of essential medicines.
But recent trial data indicate that when it's taken after unprotected sex by people who are at high risk of STIs, this workhorse antibiotic can prevent cases of chlamydia, syphilis, and gonorrhea and thus may help slow an STI epidemic in the United States that has risen sharply over the last decade.
Doxycyline post-exposure prophylaxis, or doxy-PEP, is not without its risks. Chief among them is the concern that it could promote antibiotic resistance at a time when drug-resistant infections have emerged as a looming global health crisis. But CDC officials believe that if it's used judiciously, it's the right step.
"Doxy-PEP is moving STI prevention efforts into the 21st Century," Jonathan Mermin, MD, MPH, director of the CDC's National Center for HIV, Viral Hepatitis, STD, and TB Prevention, told CIDRAP News. "This won't be the solution to the STI epidemic, but if delivered equitably, thoughtfully, and carefully, this will reduce the toll of STIs in the nation, including among people most impacted by these infections."
A highly effective intervention
The CDC has been working on the guidelines since the results of the Doxy-PEP trial were announced at the 24th International AIDS Conference in July 2022. In the trial, investigators found that, among a cohort of men who have sex with men (MSM) and transgender women (TGW) in San Francisco and Seattle who were living with HIV or were on HIV pre-exposure prophylaxis (PrEP), those who took 200 milligrams of doxycycline within 72 hours of condomless sex saw the incidence of chlamydia fall by 88%, syphilis by 87%, and gonorrhea by 55%.
The trial also found that adherence was high, with 86% of participants taking doxy-PEP consistently, and few adverse events were reported. The intervention was so successful that the trials was stopped a year earlier than planned.
"I think we were thrilled, but not completely surprised," said Stephanie Cohen, MD, MPH, director of STI and HIV Prevention and Control at the San Francisco Department of Public Health and one of the trial investigators. Cohen said she and her colleagues had seen some early efficacy data in two previous, smaller studies of doxy-PEP, and had a feeling the intervention held promise. And even before the interim data from the trial were released, they were seeing the impact in one of the clinics where they rolled out doxy-PEP.
"We could tell we were seeing fewer STIs in our study participants," she said.
This won't be the solution to the STI epidemic, but if delivered equitably, thoughtfully, and carefully, this will reduce the toll of STIs in the nation, including among people most impacted by these infections.
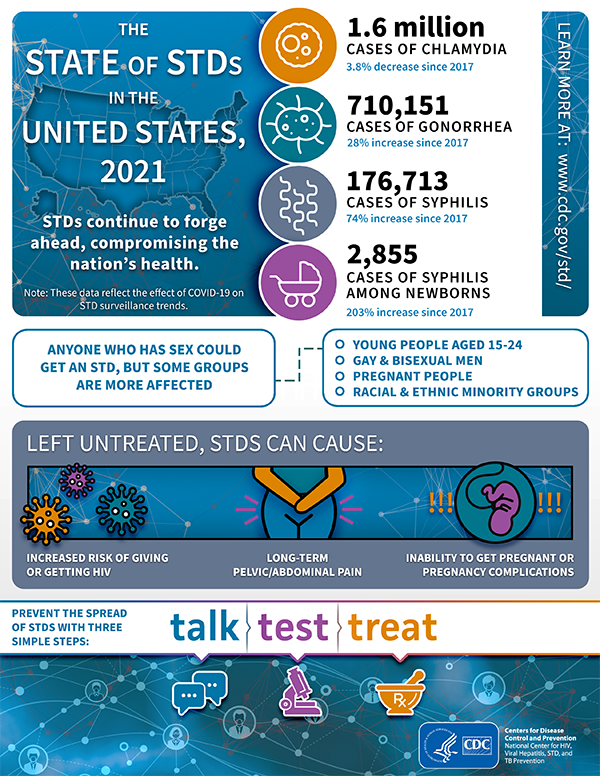
San Francisco was a good test case for the intervention because of what Cohen called a "severe epidemic" of STIs, with rates that are higher than the national average. But San Francisco is not the only US city seeing skyrocketing STI rates. From 2011 to 2021, reported STIs in the United States rose by 42%, according to the CDC. More than 2.5 million cases of chlamydia, gonorrhea, and syphilis were reported in 2021. And aside from a dip during the COVID-19 pandemic, STI rates have shown no signs of decline.
"Record high STIs threaten the health of millions of Americans," Mermin said. "We need game-changing innovations to turn the STI epidemic around."
No silver bullet
Edward Hook, MD, an STI expert and professor at the University of Alabama at Birmingham School of Medicine who is among the experts who've weighed in on the draft CDC guidelines for doxy-PEP issued earlier this year, said the inability to disrupt the upward trajectory of STIs in the country highlights the need for a new approach.
"What we've done so far hasn't worked," Hook said. "So we need something different."
Doxycycline is one of the recommended antibiotics for treating people once they've been diagnosed as having a chlamydia infections, and is an alternative for syphilis infections in patients with penicillin allergy. It's no longer used to treat gonorrhea infections. But, as Cohen explained, taking doxycycline within 72 hours of condomless sex appears to reduce the risk of those infections taking hold in people who've been exposed during sex.
"I think there is enough doxycycline exposure at the anatomic sites where one is being exposed to the infection that the bacteria cannot replicate and establish an infection," she said.
While noting that doxy-PEP isn't a silver bullet for reducing STIs, Mermin said that when implemented as part of a comprehensive sexual health framework that includes STI screening and treatment, linkage to HIV PrEP, and vaccination, it could have a substantial impact.
Potential impact on antibiotic resistance
But questions about the potential impact on antibiotic resistance are "real and concerning," according to experts who participated in a virtual meeting of the National Association of County and City Health Officials (NACCHO) in December 2022.
"We must weigh the benefits and risks of a national policy that would lead to more antibiotic use," NACCHO said in a summary report of that meeting. "Antibiotic resistance is one of our most stealthy and concerning public health threats."
The concern is that doxy-PEP could select for antibiotic resistance both in the bacteria that cause STIs as well as common bacterial pathogens, such as Staphylococcus aureus and Streptococcus pneumoniae, that reside in the anatomical sites where STIs occur and in other parts of the body.
Well aware of those concerns, investigators in the doxy-PEP trial analyzed resistance in Neisseria gonorrhoeae, other Neisseria species, and S aureus isolates collected from trial participants. There was less concern about resistance in chlamydia and syphilis because those organisms—Chlamydia trachomitis and Treponema pallidum—have not historically developed resistance to tetracyclines.
Cohen said they didn't see marked changes in antibiotic resistance at the 12-month follow-up. While the investigators did find more tetracycline-resistant N gonorrhoeae isolates in those taking doxy-PEP compared with those in the standard-of-care group (30% vs 11%), she said the clinical significance of that finding is unclear since doxycycline is not recommended for gonorrhea treatment. Doxycycline resistance in other Neisseria species didn't change much after 12 months of doxy-PEP.
Although there was a 14% absolute reduction in the number of patients in the doxycycline arm who were colonized with S aureus, there was also an 8% absolute increase in doxycycline-resistant S aureus in the doxycycline arm—a small but statistically significant increase. That could have implications, because doxycycline is sometimes used to treat methicillin-resistant S aureus skin infections. But there was not a substantial difference in doxycycline-resistant S aureus between the doxycycline group and the control group (5% vs 4%).
"We do need to continue to assess [resistance] in potentially a broader population over longer periods of time," Cohen said.
Connie Celum, MD, MPH, a co-principal investigator (PI) on the study and professor of global health, medicine, and epidemiology at the University of Washington, said monitoring for doxycycline resistance will likely have to be conducted in selected cities or clinics. That's not as easy as it sounds, she added, but will be important going forward.
"I'm an infectious disease physician, and I care about antibiotic stewardship, so I would like additional data about resistance," she said.
Mermin said the CDC is attuned to the resistance issue and committed to ensuring long-term monitoring, evaluation, and clinical studies of doxycycline resistance. He added that there will be a series of consultations with a diverse group of stakeholders to explore optimal ways to do this.
We do need to continue to assess [resistance] in potentially a broader population over longer periods of time.
Another concern raised by Hook is the potential changes to bacteria residing in the gut microbiome of people who are using doxy-PEP regularly. How gut bacteria are affected by chronic antibiotic use, and what kinds of long-term health effects that could have, has become a major topic of research in recent years.
"I don't there's any question that it's going to occur," he said. "The question is how important is it and what sort of problems is it going to cause for people."
But even with those concerns, Hook said he fully supports using doxy-PEP as a tool for STI prevention.
"I think the widespread use of antibiotics in our population is a continuing problem and a challenge," he said. "But I think within the context of all else that's going on, until something disastrous or really problematic happens, the benefits outweigh the risks."
Target population
The CDC addresses the efficacy observed in the doxy-PEP trial and previous trials, along with the potential impact on antibiotic resistance and the gut microbiome, in the draft guidelines, which looked at the risk-benefit considerations to pinpoint who would benefit most from the intervention.
"These [guidelines] have been designed to maximize the beneficial impact of doxy-PEP while minimizing antibiotic use by focusing on the groups where data suggest the most substantial impact will be achieved," Mermin said.
Based on its review of the data, the draft guidelines recommend that 200 milligrams of doxycycline within 72 hours of oral, vaginal, or anal sex "should be considered for gay, bisexual, and other MSM, and for TGW, with a history of at least one bacterial STI (i.e., gonorrhea, chlamydia or syphilis) in the last 12 months and who are at ongoing risk for acquisition of bacterial STIs." Modeling data from a study published in Clinical Infectious Diseases, Mermin noted, suggests doxy-PEP could avert 40% of STIs in these groups.

Those at-risk groups are very similar to the population that took part in the doxy-PEP trial. Cohen said it's appropriate to focus on MSM and TGW, but her concern is that limiting the recommendation to MSM and TGW who've had a documented STI in the previous 12 months could be too restrictive and could potentially worsen disparities.
"We know that some people may not have been seeking health services, may not have been diagnosed with an STI," she said. "They may know or anticipate that their risk is changing and proactively come seeking an intervention that's going to protect their health."
But the draft guidelines also suggest doxy-PEP could be considered for MSM and TGW who haven't been diagnosed as having an STI in the prior year but know that they'll be participating in activities—such as cruises and festivals—that increase their risk of STI exposure.
"I think it's a good starting point while we're trying to get experience with actually implementing it," study co-PI Celum said.
Impact on antibiotic use
How much would this strategy affect overall antibiotic use?
In a recent paper published in The Lancet Microbe, Kirstin Oliveira Roster, PhD, and Yonatan Grad, MD, PhD, of Harvard TH Chan School of Public Health, estimated that when accounting for antibiotic doses that would be averted due to prevention of chlamydia, gonorrhea, and syphilis, monthly antibiotic consumption would increase by approximately 2.52 million doses if 75% of MSM and TGW with an STI in the past year began to take doxy-PEP. That would increase to 3.36 million doses if the entire eligible population began to take it.
"Monitoring changes in antibiotic consumption, disease incidence, and burden of resistance will be important to understand the effects of doxy-PEP," they wrote.
But for Hook, if doxy-PEP is limited to those who are at highest risk of STIs, the amount of antibiotics used in that context "is a drop in the bucket compared with the amount of antibiotics used by healthcare providers for treating viral sore throats."
STI clinics and clinics that provide sexual health services in San Francisco and Seattle have already begun offering doxy-PEP to their clients. Cohen said that several thousand people have received prescriptions since her department released interim guidelines in November 2022.
On one hand, you want to make it easy to access for those who need it. But you also don't want people who don't need it to use it.
But once the CDC releases the finalized guidelines, doxy-PEP will be available at clinics throughout country. And if the efficacy observed in the doxy-PEP trial is borne out in real-world use, you could have a wider group of people seeking it out. Mermin said future research will look at the potential benefits in additional populations who experience STIs.
For Celum, whose research focuses on HIV prevention, this is where some lessons could be learned from the rollout of HIV PrEP.
"There were the early adopters, who were not necessarily the people who had the highest risk of HIV, and I think we have to be very attentive to that as we roll out doxy-PEP," she said. "On one hand, you want to make it easy to access for those who need it. But you also don't want people who don't need it to use it. So I think that's going to be a learning curve."





















