Research providing estimates of long COVID rates in Africa is scarce, and a new study published in The Lancet Global Health shows estimates across the continent vary greatly, from 2% in Ghana to 86% in Egypt.
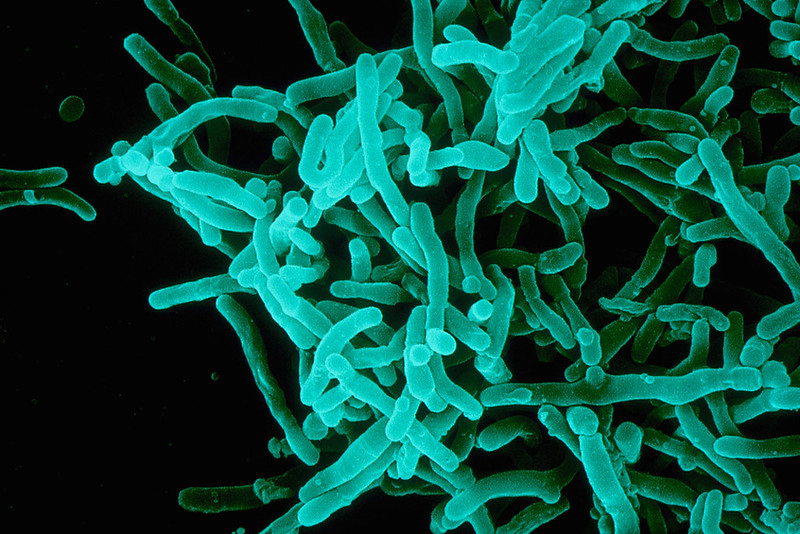
The study was based on a review of scientific literature published from December 1, 2019, through November 23, 2022, on any study type in Africa with participants who had symptoms for 4 weeks or more after an acute SARS-CoV-2 infection. The researchers identified 24 peer-reviewed manuscripts, reporting on 9,712 patients from eight African countries.
Comparing symptoms at 1-month and 3-month follow-up, one study observed a declining trend of long COVID, from 82.1% to 66.7%. The lowest prevalence—2%—was seen in a study from Ghana, and a 5% prevalence was noted in a cohort study of Ethiopian children.
Pain sensations, such as chest and muscle pain, were more frequent than respiratory symptoms, such as dyspnoea or shortness of breath.
"On the basis of reported prevalences in the included studies, the most common symptoms were neuropsychiatric symptoms, such as fatigue and headache," the authors said. "Pain sensations, such as chest and muscle pain, were more frequent than respiratory symptoms, such as dyspnoea or shortness of breath."
Low vaccination rates across continent
Three studies assessed risk factors for developing long COVID and found female sex, older age, non-Black ethnicity, and low level of education linked to the condition.
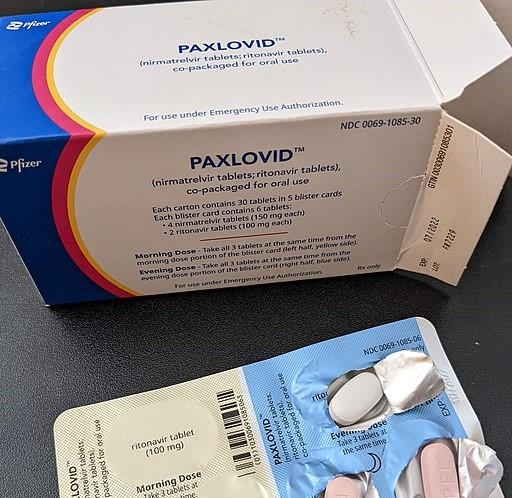
With more than 12 million long-COVID cases reported across the world, seroprevalence data suggest a pooled prevalence of 65.1% in Africa. Most cases on the continent, however, are not severe, likely because of a younger population. Africa also has low vaccination coverage, the authors said, and the studies included in this review occurred when 0.1% of the population had been vaccinated against COVID-19.
"In Africa, where vaccine coverage is low, the findings of this review should reignite discussions on the true toll of COVID-19 on the continent and guide advocacy and policy efforts to scale up effective interventions, including for vaccine uptake," the authors conclude.