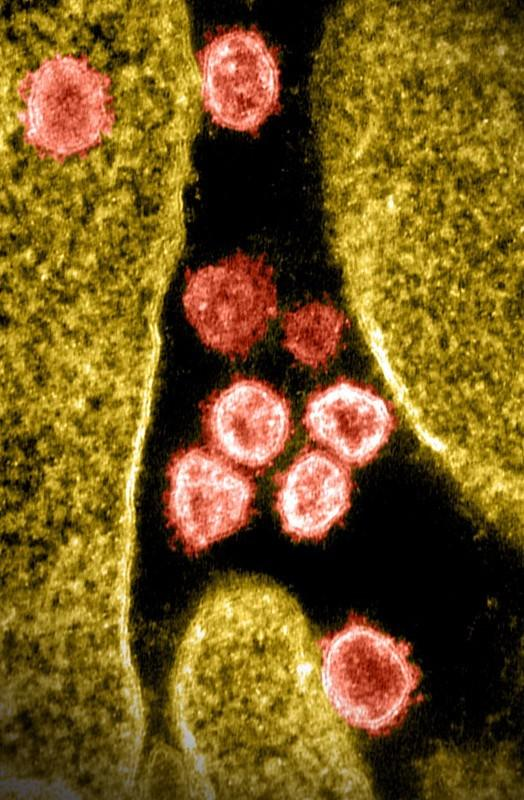
Infection with the SARS-CoV-2 Omicron variant confers weak, short-term protection against reinfection, compared with the much more robust and durable protection provided by earlier variants, which highlights the need for periodic vaccine updates, a Cornell University Qatar–led study suggests.
The researchers used a test-negative, case-control study design to compare the efficacy of SARS-CoV-2 Omicron infection against reinfection and poor outcomes in Qataris with that offered by infection with previously dominant strains such as Alpha, Beta, and Delta. COVID-positive people were matched with COVID-negative controls in a 1:2 ratio by sex, age-group, nationality, number of underlying medical conditions, vaccine doses received, week of COVID-19 test, testing method, and reason for testing.
The results were published yesterday in Nature.
"The arrival of the Omicron variant marked a major shift, introducing numerous extra mutations in the spike gene compared with earlier variants," the study authors wrote. "These evolutionary changes have raised concerns regarding their potential impact on immune evasion, disease severity and the effectiveness of vaccines and treatments."
Protection after pre-Omicron infection
The estimated effectiveness of a pre-Omicron infection in preventing reinfection with a pre-Omicron strain was 81.1%, regardless of symptoms. The median interval between the previous infection and the study COVID-19 test was 252 days.
The estimated effectiveness against symptomatic reinfection with a pre-Omicron strain was 86.8%, with no evidence of waning over time. The median interval between infection and the study COVID-19 test was 244 days. Subgroup analyses by vaccination status yielded comparable results.
The effectiveness of a pre-Omicron infection against severe, critical, or fatal COVID-19 on reinfection with a pre-Omicron strain was 98.0%, with no waning over time after infection.
Lower protection with Omicron
The protection against symptomatic or asymptomatic reinfection conferred by natural infection by Omicron, however, which emerged in late 2021, was 53.6%. The median interval between the previous infection and the study COVID-19 test was 245 days.
During the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.
Effectiveness rapidly declined after the previous infection, dropping from 81.3% at 3 to 6 months to 59.8% in the next 3 months and 27.5% in the 3 months after that. Protection was negligible after 1 year. Efficacy was 59.5% in the first year, plummeting to 4.8% thereafter.
Overall effectiveness against symptomatic reinfection was 45.4%, declining rapidly thereafter. The median interval between the previous infection and the study COVID-19 test was 301 days. Effectiveness of Omicron infection in preventing severe, critical, or fatal COVID-19 after reinfection with Omicron was 100%. There was no evidence for waning effectiveness after previous infection.
Host immunity, viral evolution
"Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time," the researchers wrote. "However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year."
The findings show that COVID-19 immunity is shaped by a dynamic interaction between host immunity and viral evolution, they said. "This shift in patterns suggests a change in evolutionary pressures, with intrinsic transmissibility driving adaptation pre-Omicron and immune escape becoming dominant post-Omicron, underscoring the need for periodic vaccine updates to sustain immunity," they wrote.
The shift is likely the result of a complex interplay of multiple factors in addition to waning immunity, immune evasion, and the accelerated and convergent evolution of Omicron, such as immune imprinting, varying immunogenicity, global population immunity, and population characteristics tied to infection in different phases of the pandemic.
Differences in protection against reinfection may stem from distinct evolutionary pressures acting on SARS-CoV-2 before and after the emergence of Omicron, the authors said: "In the pre-Omicron era, with a large proportion of individuals remaining immune naive because of non-pharmaceutical interventions and delayed scale-up of vaccination, intrinsic transmissibility may have been the primary driver of viral adaptation."
"Conversely, following the very large and widespread Omicron wave in early 2022…most individuals possessed some level of immunity, either from infection or vaccination," they added. "This may have shifted the dominant evolutionary pressure towards immune escape through not only antigenic drift, but also recombination and convergent evolution as the adaptive mechanisms for the virus."
The findings underscore the dynamic interaction between viral evolution and host immunity, which the researchers said highlights the need for continued monitoring and periodic vaccine updates to restore immunity and counter viral immune evasion.