A University of Colorado–led case report in Emerging Infectious Diseases, describes a 58-year-old woman who, an estimated 48 years after treatment with cadaver-derived human growth hormone, died of iatrogenic Creutzfeldt-Jakob disease (iCJD), a prion disease.
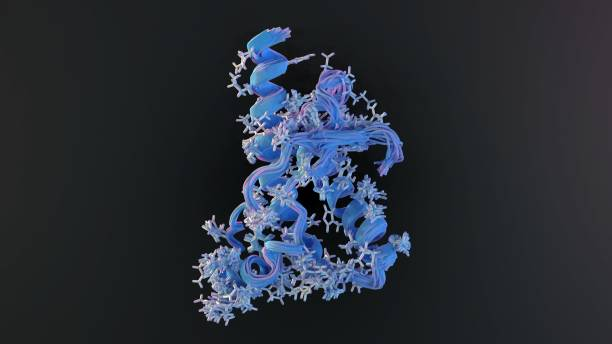
The patient, who sought care after developing gait imbalance and tremors 2 weeks earlier, had received prion-contaminated cadaveric human growth hormone (chGH) for 9.3 years starting at age 7. Prion diseases, which affect both humans and animals, are fatal neurologic conditions caused by infectious misfolded proteins.
chGH is a well-described iatrogenic (healthcare-related) cause of this type of CJD. The National Hormone Pituitary Program (NHPP) administered the drug to treat growth failure to roughly 7,700 US patients from the 1960s through the 1980s, the researchers noted. An outbreak of chGH-related iCJD, first recognized in the United States in 1985, prompted the immediate shutdown of chGH production and NHPP administration of the drug.
Soon after, chGH was replaced with recombinant (biosynthetic) human growth hormone, but the iCJD outbreak continued due to the often-long latency period in some previous chGH recipients. Latency periods for prion diseases are variable and depend on factors such as the infectious particle dose (higher doses are linked to shorter latency); route of infection (central nervous system [CNS] exposures are tied to shorter latency than peripheral ones); and recipient genetics, particularly the codon 129 polymorphism in the PRNP gene.
iCJD is more of a public health concern than the other two CJD types—sporadic and genetic—because of its potential to cause outbreaks.
Rapid clinical deterioration
This patient was the 36th iCJD case among US NHPP chGH recipients and the 254th such case worldwide as of January 2024.
When she presented for treatment, her medical history included depression, cervical spine fusion, and idiopathic panhypopituitarism, a condition that occurs when the pituitary gland doesn't produce all or most of its hormones, but it isn't clear why. The initial neurologic exam showed frequent lateral movements of the head and trunk, as well as irregular hand movements that went away with distraction, but the exam was otherwise unremarkable.
Magnetic resonance imaging (MRI) of the brain and cervical spine revealed no pathology. Results of the Mayo Clinic Autoimmune Movement Disorders Panel and HIV screening were negative, and copper, vitamin E, and vitamin B12 levels were within normal ranges. The patient was referred to the movement disorders clinic and advised to start physical therapy and continue psychologic treatment.
Over the next month, the patient developed urinary incontinence, worsening tremors, decreased speech, and abnormal gait. She returned to the hospital with tachypnea (abnormally fast breathing), hyperekplexia (exaggerated startle reflex with intense muscle stiffness), and appendicular rigidity (stiffness in the arms and legs).
Her breathing and alertness quickly declined, and she was intubated. In the next several days, she developed both stimulus-induced and spontaneous myoclonus (a neurologic condition featuring sudden, involuntary muscle jerks or twitches), and she remained in a coma.
Positive prion assay, death
A repeat brain MRI 2 months after the initial exam revealed lesions, and continuous electroencephalography showed frequent 1- to 2.5-Hertz generalized periodic discharges of 3 to 9 seconds.
The woman's antinuclear antibody level was mildly positive, but all other serum test results, including for autoantibodies, generated no pathologic findings. Cerebrospinal fluid (CSF) viral and autoantibody test results were negative. Oligoclonal bands (proteins in the CSF that can indicate CNS inflammation or damage) were absent.
Prion testing at the National Prion Disease Pathology Surveillance Center (NPDPSC) at Case Western Reserve University showed substantially elevated total tau (protein that forms tangles in the brain) and a very high concentration of 14-3-3 protein. A real-time quaking-induced conversion assay was positive for prions. Per the patient's documented wishes, she was extubated and died.

An autopsy performed at NPDPSC confirmed CJD via Western blot and immunohistochemistry analysis of brain tissue. An examination of the PRNP gene, which is involved in genetic CJD, was negative for pathogenic mutations, supporting a diagnosis of iCJD in the context of previous chGH treatment.
The patient had a methionine/valine polymorphism (change in the DNA sequence that is common in a population) at codon 129 of the PRNP gene, which has been tied to longer incubation periods in acquired human prion diseases.
Difficult to estimate latency
Determining the precise latency period for chGH-linked iCJD cases is often impossible, because patients were often exposed to chGH for many years, the researchers said. But it can be estimated using the interval from the first dose of chGH and iCJD symptom onset, the period from the midpoint of chGH treatment to iCJD symptom onset, the time between the last dose of chGH and symptom onset, and the midpoint of chGH treatment calculated from the first chGH dose to the end of 1977.
Of note, none of the 36 US iCJD cases exclusively received post-1977 chGH, likely because the NHPP developed a new laboratory method to extract chGH from pituitary glands in 1977.
"The reason for considering that method of calculation involves the epidemiology of the US outbreak, which suggests that the most likely source of iCJD infection came from chGH administered before or during 1977, even though most of the ≈7,700 NHPP recipients started chGH treatment after 1977," the authors wrote.
"Of note, none of the 36 US iCJD cases exclusively received post-1977 chGH, likely because the NHPP developed a new laboratory method to extract chGH from pituitary glands in 1977," they added. "That method included column purification to separate and collect multiple hormones from the glands, a procedure now known to have greatly reduced prion contamination."
New outbreak cases still possible
For this study, the team performed all four latency estimate calculations: "First dose of chGH to symptom onset was 51.3 years, midpoint of chGH treatment to symptom onset was 46.7 years, last dose of chGH to symptom onset was 42.1 years, and midpoint of pre-1978 chGH to symptom onset was 48.3 years. We compared our patient’s latency estimate calculation to all US chGH-associated iCJD cases, and given the evidence implicating pre-1978 chGH, we considered the final method to provide the most accurate estimate of 48.3 years latency."
Clinicians should recognize the continued possibility of chGH-associated CJD cases and include iCJD in the differential diagnosis for anyone with new neurologic symptoms and prior chGH exposure, particularly patients exposed to chGH before the 1977 updated purification process.
The estimated latency of the ongoing US chGH-related iCJD outbreak was 10 years, compared with 5 years among the first 226 cases reported internationally, which the authors said suggests a lower level of prion contamination in US NHPP-distributed chGH.
Also, experimental transmission studies in nonhuman primates using samples of all 76 lots of chGH retained at the US NHPP demonstrated that prion contamination was rare and random. "That low level of contamination, the purification step introduced in the United States in 1977, and the peripheral route of administration created an environment that would be expected to result in longer latency periods," the investigators noted.
While the US iCJD outbreak has slowed considerably, new cases are still possible, particularly among chGH recipients who are heterozygous M/V at codon 129 of the PRNP gene. "Clinicians should recognize the continued possibility of chGH-associated CJD cases and include iCJD in the differential diagnosis for anyone with new neurologic symptoms and prior chGH exposure, particularly patients exposed to chGH before the 1977 updated purification process," they concluded.



















