Anticoagulation therapy given to prevent or treat venous thromboembolism (VTE) was linked to lower death rates in hospitalized adult COVID-19 patients, but the association remained at 60 days only for the prophylactic (preventive) strategy, according to a multicenter study today in JAMA Network Open.
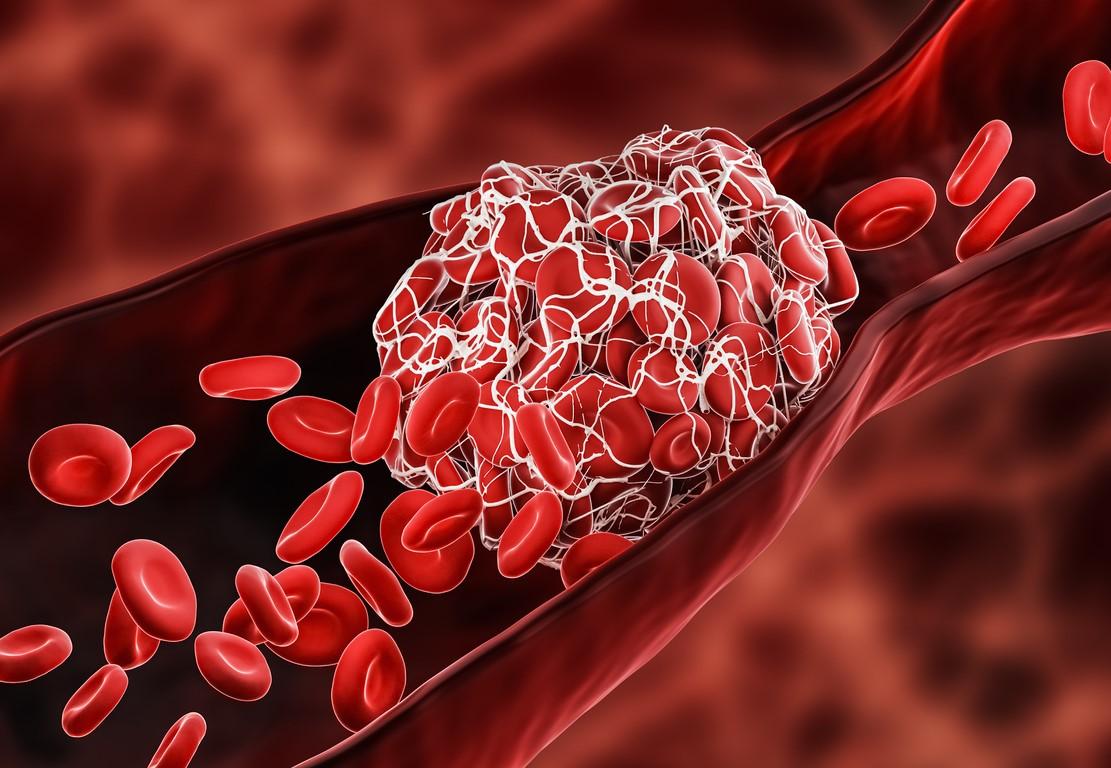
The study, led by University of Utah and University of Michigan researchers, involved a pseudorandom sample of 1,351 COVID-19 patients 18 years and older admitted to 30 Michigan hospitals from Mar 7 to Jun 17, 2020. VTE, or blood clots that cause a blockage in the veins, is a leading complication of COVID-19, the authors noted.
Compared with no anticoagulation, any dose of anticoagulation was tied to lower in-hospital death rates (aHR for prophylactic dose, 0.36; aHR for treatment dose, 0.38). But only the preventive dose was still associated with lower death rates at 60 days (aHR for prophylactic dose, 0.71; aHR for treatment dose, 0.92).
Of the 1,351 patients, 1,127 (83.4%) received anticoagulation (eg, heparin, enoxaparin) at some point in their hospital stay. Only 162 patients (12.0%) received no anticoagulation, either because they were deemed at low risk or had contraindications to treatment.
Forty-eight patients (3.6%) were diagnosed as having VTE. Eighteen (1.3%) had confirmed VTE 2 days after admission, while 219 (16.2%) received treatment doses of anticoagulation for a median of 5 days. None of the patients in the no-anticoagulation group had VTE by 60 days, while 1.7% of the prophylactic-dose group and 14.6% of the treatment-dose group had VTE in that timeframe.
In-hospital, 60-day mortality
Zero to 29% of hospitals used treatment doses of anticoagulants without imaging, but their use rose over time, from 4% in the first week to 57% by week 13 (adjusted odds ratio [aOR], 1.46 per week).
The in-hospital death rate for all patients was 18.3% (41.1% of patients requiring intensive care vs 8.4% receiving standard care), and 23.2% died within 60 days of hospitalization (45.0% vs 13.7%).
In-hospital deaths occurred in 12.4% of patients who did not receive anticoagulation, compared with 15.8% of the group given prophylactic doses. And 14.2% of patients not given anticoagulants, 39.7% of those receiving treatment doses, and 20.9% of the prophylactic dose group died within 60 days. COVID-19 was the cause of death in 67.7% of cases, while 1.3% were attributed to VTE.
Among the 1,127 patients given anticoagulation, 392 (34.8%) missed at least 2 days of prophylactic therapy. Missed preventive anticoagulant doses ranged from 11% to 61% across hospitals and declined with time (aOR, 0.89 per week). Missed doses were linked to higher death rates at 60 days (adjusted hazard ratio [aHR], 1.31) but not to higher in-hospital death rates (aHR, 0.97).
More intense anticoagulation was typically given to older patients (median age of those receiving treatment doses, 66 years vs 57 years in the no-anticoagulant group) and those with longer hospitalizations (median length of stay, 10 vs 5 days), more underlying illnesses (median Charlson comorbidity score, 2 vs 1), more severe disease (58% vs 26.6% received intensive care), receipt of more COVID-19 treatments (eg, 53.1% vs 12.1% received corticosteroids), and more inflammatory markers.
Median patient age was 64 years, 47.7% were women, 48.9% were Black, and 40.0% were White. Median length of hospital stay was 6 days, and 409 patients (30.3%) required intensive care.
Preventive doses for all hospitalized COVID patients
"This large, multicenter cohort of patients hospitalized with COVID-19, found evidence of rapid dissemination and implementation of anticoagulation strategies, including use of treatment-dose anticoagulation," the researchers concluded. "As only prophylactic-dose anticoagulation was associated with lower 60-day mortality, prophylactic dosing strategies may be optimal for patients hospitalized with COVID-19."
In a commentary in the same journal, Andrew Dicks, MD, and Ido Weinberg, MD, both of Massachusetts General Hospital, said that the study was limited by its study design, lack of sufficient detailed data (eg, bleeding rate), and possible deficient matching.
However, they wrote, "Despite the limitations, this study (especially in the context of other published data) should make clinicians more confident that the use of prophylactic anticoagulation is warranted for hospitalized patients with COVID-19, as currently suggested by published societal guidelines."
"We eagerly await randomized trial data," Dicks and Weinberg added, "while secretly hoping that by the time these are published we will have little need for their conclusions."