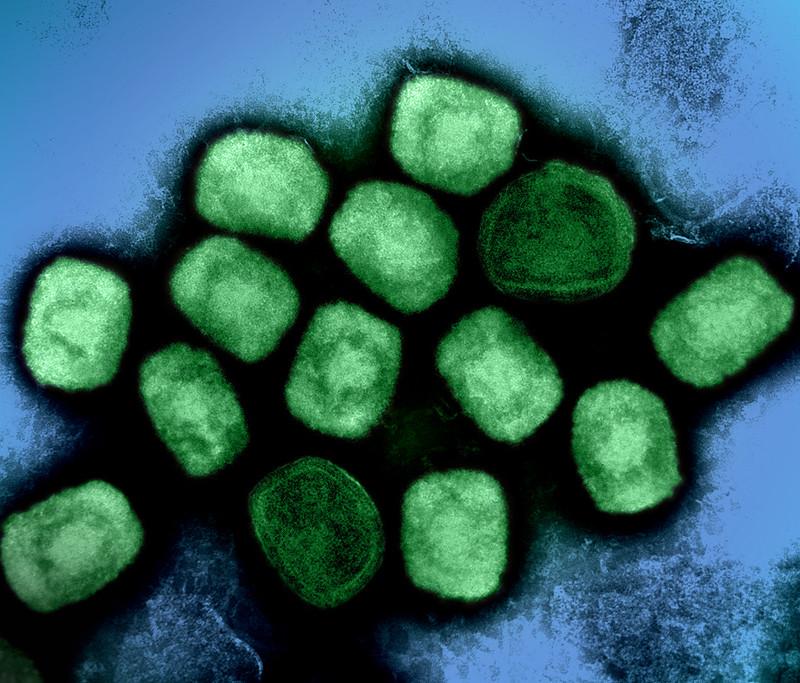
Swiss biotech company LimmaTech Biologics AG announced late last week that the US Food and Drug Administration (FDA) has granted Fast Track authorization to the company's Staphylococcus aureus vaccine candidate.
The multivalent toxoid vaccine, LBT-SA7, contains weakened forms of multiple S aureus toxins, and is designed to prevent skin and soft-tissue infections (SSTIs) caused by the pathogen. SSTIs account for roughly 90% of all S aureus infections and can vary from superficial wound infections to more severe, virulent infections, especially when caused by methicillin-resistant S aureus.
"Staphylococcus aureus infections are a major cause of global mortality and morbidity, with traditional antibiotic treatments becoming increasingly ineffective due to rising antibiotic resistance," LimmaTech CEO Franz Werner-Haas said in a company press release. "Despite this urgent medical need, no vaccine is currently available to prevent the consequences of an S. aureus infection."
The FDA's Fast Track designation expedites the review process for products that have the potential to treat or prevent serious conditions and address unmet medical needs.
The company says the safety and immunogenicity of LBT-SA7 will be tested in a phase 1 clinical trial in the United States involving 130 participants aged 18 to 50 years, with initial results reported in the second half of 2025.