A large genomic study of the gut microbiome suggests that antibiotic use is not the only factor contributing to the spread of antimicrobial resistance (AMR) in the population.
The authors of the study, which was presented at this week's European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Copenhagen, Denmark, say the findings indicate that other medications, along with geography, demographics, and diet, also play a role.
Resistance gene abundance, diversity
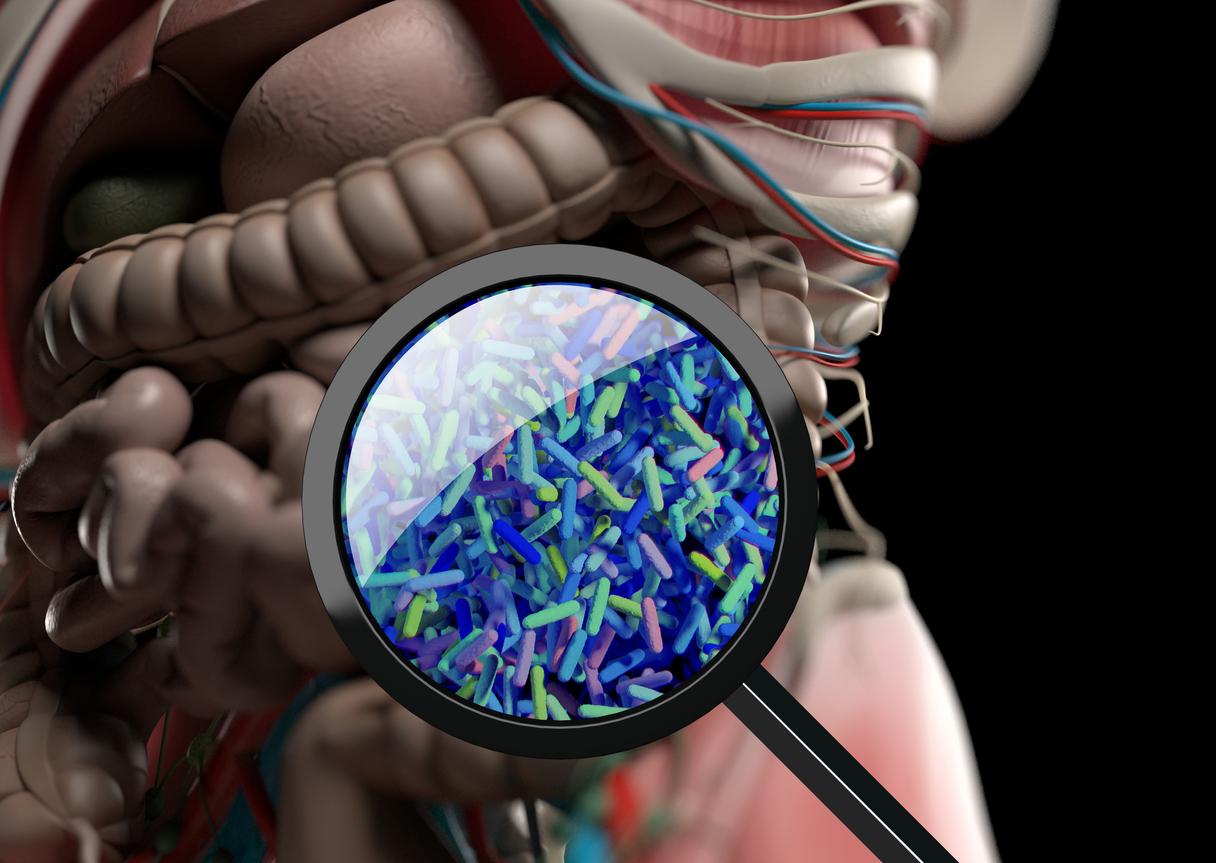
In the study, a team led by researchers at the University of Turku in Finland performed shotgun metagenomic sequencing on fecal samples from 7,098 healthy Finnish adults taking part in the FINRISK study, a population-based survey carried out every 5 years. Shotgun metagenomic sequencing involves taking the DNA out of all the bacteria in the samples, breaking it into small pieces, and analyzing all of the pieces for the presence of antibiotic resistance genes (ARGs).
The aim of the study, which adds to a growing body of research on resistance genes in the gut microbiome and the role they may play in the spread of AMR, was to determine ARG abundance, composition, and diversity and examine associations with FINRISK data. Since 1972, the FINRISK study has collected information on the health, lifestyle, diet, and medication use of Finnish adults for use in a variety of different research projects.
Our findings clearly show that geography, demographics, and diet play an underappreciated role in antibiotic resistance.
Not surprisingly, antibiotic use was linked to higher ARG loads. But use of psycholeptic drugs (including opioids and barbiturates) was also positively correlated with higher ARG abundance. The analysis also found that more frequent consumption of raw vegetables and poultry was associated with higher ARG loads and diversity.
In addition, people living in western Finland had more ARGs and more diverse microbiomes, as did people living in more densely populated areas of the country. Women and people in upper-income brackets also had more ARGs.
"Our findings clearly show that geography, demographics, and diet play an underappreciated role in antibiotic resistance," lead study author Katariina Parnanen, PhD, of the University of Turku, said in an ECCMID press release. "This has important implications for the antibiotic resistance crisis as more and more people are living in densely populated areas and cities and are able to buy more expensive types of foods, such as meat, and fresh produce, and also medication."
Parnanen says the findings suggest national actions plans to address AMR will require more than regulating antibiotic use.