Three new studies in Emerging Infectious Diseases report mostly positive responses to newer treatments for multidrug-resistant and extensively drug-resistant tuberculosis (MDR- and XDR-TB).
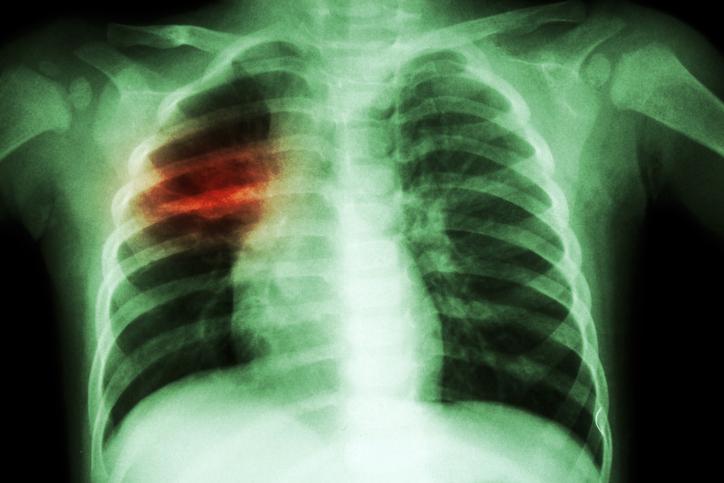
The two drugs studied are bedaquiline, which works by blocking an enzyme inside the Mycobacterium tuberculosis bacteria called ATP synthase, and delamanid, which inhibits mycolic acid synthesis. Both drugs are for the treatment of MDR-TB that is affecting the lungs, and are used only when other TB drug combinations cannot be used because of resistance or side effects.
Bedaquiline was approved by the US Food and Drug Administration (FDA) in 2012, and the World Health Organization (WHO) issued guidance on use of the drug in 2013; Delamanid received conditional approval from the European Medicines Agency in 2014, and the WHO issued guidance for use in the same year.
While TB is curable when patients adhere to the treatment regimen, MDR-TB and XDR-TB are much more difficult to treat. Treatment options are limited, expensive, and often toxic, and the drug regimens can last for up to 2 years. Delamanid and bedaquiline "represent hope for better outcomes," one of the studies notes.
Three small studies on efficacy, safety
In the largest of the three studies, published today, researchers presented findings on interim treatment response and safety response in 53 patients from seven countries treated with delamanid from Feb 6, 2015, to Feb 29, 2016. Most patients had been treated previously with second-line drugs (48/53, 90.6%), experienced MDR-TB treatment failures (32/53, 60.4%), exhibited resistance to second-line TB drugs (41/51, 80.4%), or had extensive pulmonary disease (40/45, 88.9%).
After 6 months of treatment, 67.6% (25/37) of the patients who were culture positive at the start of delamanid treatment had culture converted (defined as two consecutive negative culture results 1 month apart). Thirty-nine of 53 patients (73.6%) had a favorable response to treatment, 13.2% (7/53) had died, 7.5% (4/53) remained culture positive, and 1.9% (1/53) had failed treatment because of a serious adverse event (SAE).
A total of 31 SAEs were reported in 14 patients (26.4%). The most common were hepatoxicity, electrolyte imbalance, and QT prolongation—a syndrome that causes irregular heart rhythms. Causes of the seven reported deaths were advanced TB in two of the patients, encephalitis in an untreated HIV patient, traumatic pneumothorax, sepsis in an HIV patient, respiratory failure related to end-stage hepatitis, and sudden death of an unknown cause.
The authors of the study, which was led by researchers from Medecins Sans Frontieres (MSF, or Doctors Without Borders), said the preliminary results indicate good tolerability and interim treatment response in a "narrow and difficult-to-treat cohort of patients."
In the second-largest study, published yesterday, researchers collected data from November 2014 through January 2017 on 27 children and adolescents being treated with bedaquiline at TB treatment programs supported by MSF in South Africa, Tajikistan, and Uzbekistan. Of the 27 children, 67% (18/27) had XDR-TB, 22% (6/27) had MDR-TB with fluoroquinolone resistance, and 11% (3/27) had MDR-TB with resistance to a second-line injectable drug.
Overall, 27 children completed 24 weeks of bedaquiline therapy. As of Feb 24, 2017, of the 23 patients that remained on treatment and had data available, all were culture negative, and no clinical signs of treatment failure were noted. Five of the children reported grade 3 or 4 adverse effects caused by bedaquiline (QT prolongation), but no patients required bedaquiline cessation.
The findings are significant because to date there has been limited pharmacokinetic data available to inform the use of bedaquiline in children. As a result, the WHO has recommended against the use of the drug in children.
"Our experience suggests that bedaquiline can be used safely in children >12 years of age with appropriate monitoring and could be considered in younger children in select circumstances when benefits are likely to outweigh risks," the authors write.
Combination treatment
In the smallest of the three studies, researchers investigated co-administration of bedaquiline and delamanid, which the WHO also recommends against due to lack of evidence regarding safety. Public health officials are concerned that co-administration of the two drugs could increase the occurrence of adverse events.
In the retrospective observational study published yesterday, the researchers looked at five patients with culture-confirmed XDR-TB from the International Bedaquiline Study Group who had been treated with a combination of bedaquiline and delamanid from 2008 through 2016. All had previously been treated with TB drugs, and four of those patients had drug treatment failures.
As of Apr 28, 2017, one patient had been cured, three patients were continuing therapy, and one patient with additional resistance to other TB drugs had died. Two of the patients had potentially life-threatening QT prolongation but no arrhythmias.
"Although these data are preliminary and more work is needed, the findings from this cohort suggest that providing bedaquiline and delamanid in combination as part of therapy against XDR-TB is justified when clinical options are limited," the authors write.
The WHO estimates that 480,000 cases of MDR-TB occurred globally in 2015, and that at least 10% of those cases were XDR-TB or totally drug-resistant TB.
See also:
Aug 1 Emerg Infect Dis research letter
Jul 31 Emerg Infect Dis study on bedaquiline in children
Jul 31 Emerg Infect Dis study on combo drug therapy