A randomized clinical trial in the United Kingdom found that a procalcitonin-guided algorithm did not reduce the duration of intravenous (IV) antibiotics in hospitalized children compared with usual care, researchers reported last week in The Lancet Child & Adolescent Health.
The BATCH (Biomarker-guided duration of Antibiotic Treatment in Children Hospitalised) trial, led by investigators from UK universities and hospitals, enrolled children aged 72 hours to 18 years who were treated with IV antibiotics for suspected or confirmed bacterial infection at 15 hospitals. Of the 15,282 children screened from June 11, 2018, to October 12, 2022, 1,949 (median age, 3.1 years; 54% male) were randomly assigned to receive procalcitonin-guided therapy (977 children) or usual care (972). The co-primary outcomes were duration of antibiotic use (assessed for superiority) and a composite safety measure (assessed for non-inferiority).
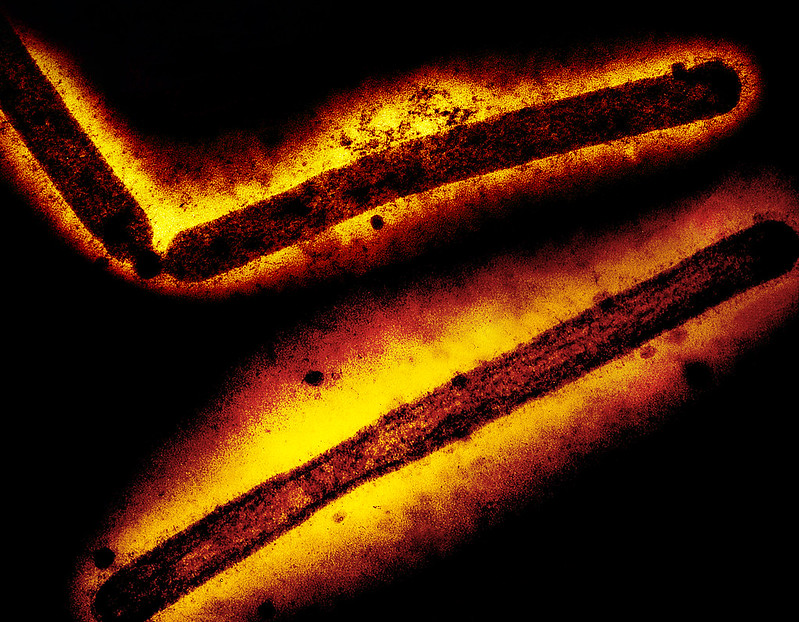
The aim of the trial was to investigate whether the use of procalcitonin, a biomarker for bacterial infection, would safely reduce antibiotic duration compared with usual care, in which C-reactive protein is used to guide antibiotic therapy. The investigators hypothesized that because procalcitonin is a more specific host-response biomarker for bacterial infection, it might better facilitate decisions to de-escalate antibiotic therapy.
No evidence of treatment effect
But the results did not support that theory. The median IV antibiotic duration was 96 hours in the procalcitonin group and 99.7 hours in the usual care group (hazard ratio, 0.96; 95% confidence interval [CI], 0.87 to 1.05), providing no evidence of a treatment effect. Comparison of safety outcomes showed 9% of children in the procalcitonin group and 9% in the usual-care group had at least one event covered by the composite safety outcome measure (estimated adjusted risk difference, -0.81), indicating procalcitonin-guided therapy was non-inferior to usual care.
Investigators also found that total costs were higher in the procalcitonin group, and that adherence to the protocol was low.
"Our results suggest that in hospitalised children treated with intravenous antibiotics for suspected or confirmed serious bacterial infection, a procalcitonin-guided algorithm is not effective in reducing intravenous antibiotic duration, especially where robust antimicrobial stewardship programmes are already implemented," they concluded.