 A systematic review and meta-analysis found that rapid point-of-care testing for respiratory pathogens does not reduce the antibiotic prescribing rate, Finnish researchers reported late last week in Open Forum Infectious Diseases.
A systematic review and meta-analysis found that rapid point-of-care testing for respiratory pathogens does not reduce the antibiotic prescribing rate, Finnish researchers reported late last week in Open Forum Infectious Diseases.
Out of 754 abstracts screened, the researchers analyzed 10 randomized controlled studies involving 7,323 patients that compared the impact of rapid point-of-care viral and/or bacterial polymerase chain reaction (PCR) tests on antibiotic prescribing for acute respiratory infections regardless of the blinding and comparator. Four of the studies analyzed influenza and respiratory syncytial virus (RSV) tests, and six analyzed multiplex (viral and/or bacterial) tests. The primary outcome was the antibiotic prescribing rate.
Overall, the antibiotic prescribing rate was 52.7% in the testing group and 54.6% in the control group (risk ratio [RR], 0.99; 95% confidence interval [CI], 0.96 to 1.01), with evidence quality ranked as moderate. When the researchers analyzed the influenza + RSV testing group, the prescribing rate was 48.2%, compared with 48.7% in the control group (RR, 0.97; 95% CI, 0.92 to 1.02). The prescribing rate in the multiplex testing group compared with the control group was 54.3% versus 57.3% (RR, 1.00; 95% CI, 0.96 to 1.04).
In an age-stratified analysis of the three studies that included children and five adults-only studies, the antibiotic prescribing rates showed no evidence of a difference (children RR, 1.03; 95% CI 0.81 to 1.30; adults RR, 0.98; 95% CI, 0.96 to 1.01). Analysis of five studies that compared antibiotic duration found no evidence that duration was shorter in the testing group.
Non-medical factors may play a role
The study authors say the findings are consistent with previous studies and suggest that non-medical factors, such as patient preference and physician attitude, may also play a role in antibiotic prescribing for respiratory illnesses.
"Further strategies and studies are needed to provide evidence-based interventions for antibiotic prescription reduction," they wrote.
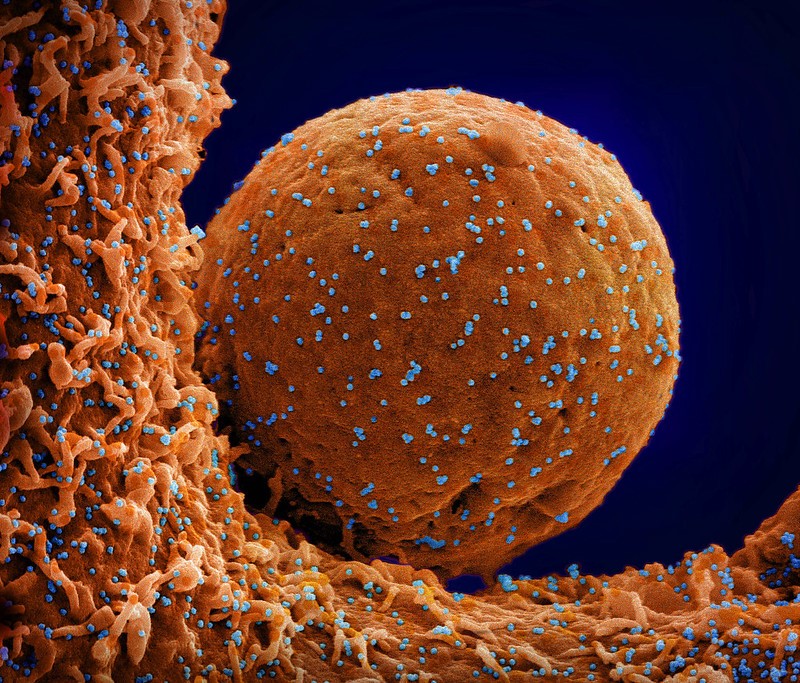
 Early in the COVID-19 pandemic,
Early in the COVID-19 pandemic, 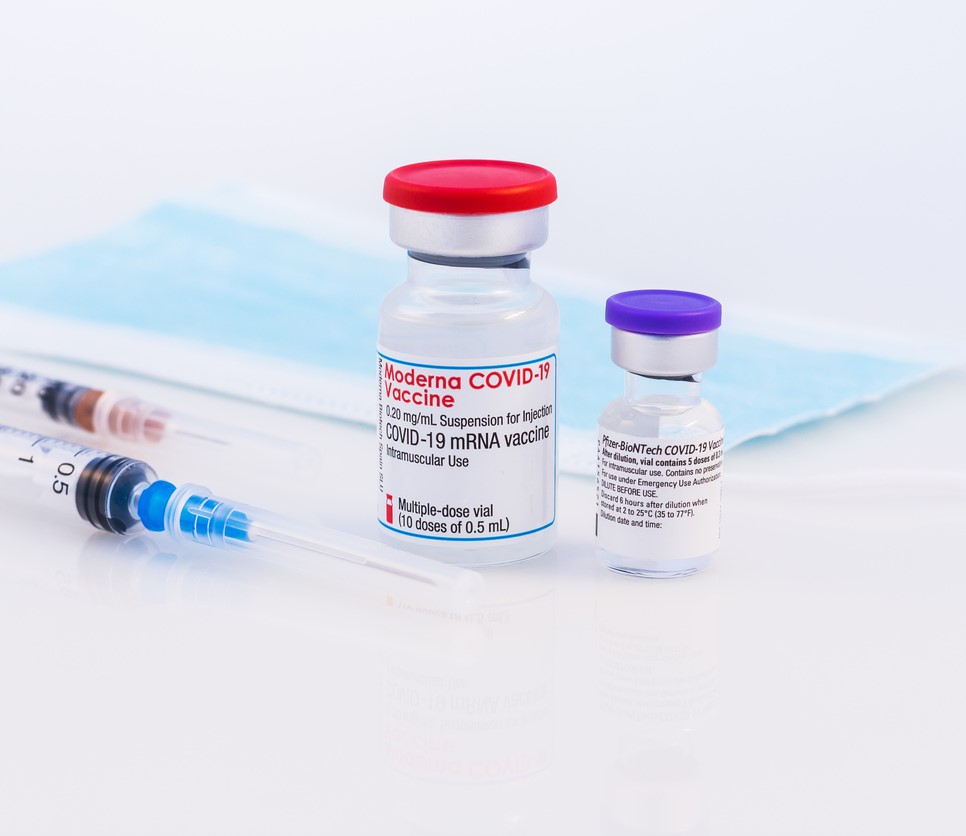 COVID-19 infections among 2,400 vaccinated transplant recipients were common (19.7%) during SARS-CoV-2 Omicron variant predominance in the United States, but only 7.5% needed hospitalization, estimates a
COVID-19 infections among 2,400 vaccinated transplant recipients were common (19.7%) during SARS-CoV-2 Omicron variant predominance in the United States, but only 7.5% needed hospitalization, estimates a 













