The results of a large observational study suggest fluoroquinolone antibiotics are associated with an increased short-term risk of aortic aneurysm.
The study, published yesterday in JAMA Surgery, found that aortic aneurysm incidence within 90 days of filling a fluoroquinolone prescription was 20% higher in adults 35 and over compared with other antibiotics.
In particular, there was a 31% higher incidence of abdominal aortic aneurysm and a 61% higher incidence of iliac artery aneurysm after fluoroquinolone use. Overall incidence of aneurysm in the cohort of more than 27 million Americans was low.
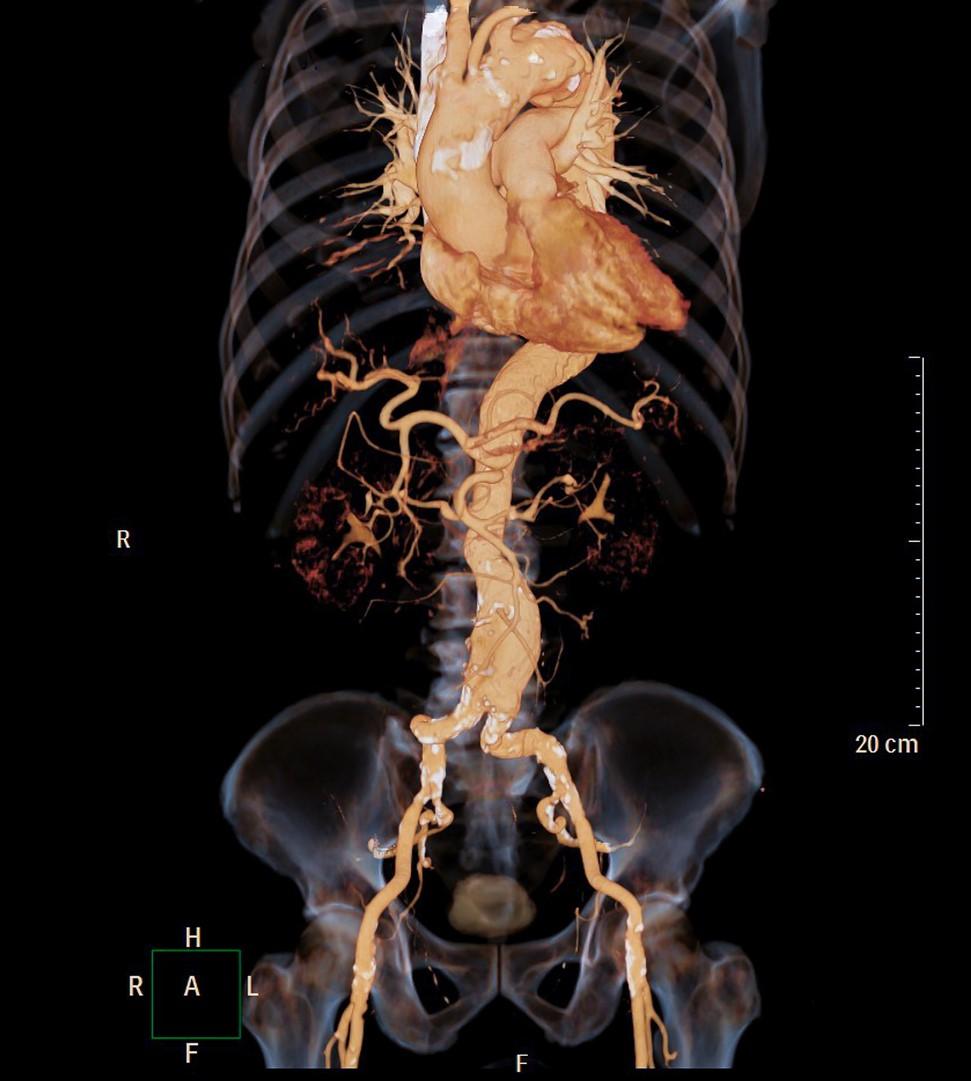
The Food and Drug Administration (FDA) added to its black box warnings on fluoroquinolones in 2018 to advise that people with a history of aortic aneurysm—a balloon-like bulge in the aorta that can cause life-threatening internal bleeding if it ruptures—or blockages of other blood vessels, or high blood pressure should consider alternative antibiotics. The warning was based on an FDA review of studies showing fluoroquinolones were associated with an increased risk of aortic aneurysm or dissection (a tear or separation in the lining of the aorta).
"For patients who have an aortic aneurysm or are known to be at risk of an aortic aneurysm, we do not believe the benefits outweigh this risk, and alternative treatment should be considered," the FDA wrote.
But the authors of the study say these findings indicate that fluoroquinolones, which are one of the most commonly prescribed antibiotic classes in the United States and are used for a variety of bacterial infections, should be used with caution not just in high-risk groups but in all adults 35 and over.
Increased aneurysm incidence
In the study, researchers from the University of North Carolina analyzed health insurance claims data from a large commercial database, looking at all prescription fills for fluoroquinolones or a comparator antibiotic (amoxicillin-clavulanate, azithromycin, cephalexin, clindamycin, and sulfamethoxazole-trimethoprim) among adults aged 18 to 64 years from Jan 1, 2005 through Sep 30, 2017.
They then followed these adults for 90 days after the antibiotic fill date. Individuals with a pre-existing diagnosis of aneurysm or dissection were excluded. The primary outcome was 90-day incidence of aneurysm and aortic dissection per 10,000 antibiotic fills.
The cohort study included 27.8 million people with 47.6 million antibiotic episodes. Fluoroquinolones accounted for 19% of prescription fills, and comparator antibiotics accounted for 81%. Adults prescribed fluoroquinolones had a median age of 47 years, compared with a median age of 43 years in the comparator group.
A total of 24,141 aneurysm events were diagnosed within 90 days of a fluoroquinolone or comparator antibiotic fill. The unweighted incidence of aneurysm (including dissection) in the fluoroquinolone group was 7.5 cases per 10,000 fills versus 4.6 cases per 10,000 fills in the comparator group. After weighting for demographic characteristics and comorbidities, fluoroquinolones were still associated with a significant increase in aneurysm incidence compared with other antibiotics (hazard ratio, [HR], 1.20; 95% confidence interval [CI], 1.17 to 1.24).
More specifically, fluoroquinolones were associated with increased 90-day incidence of abdominal aortic aneurysms (HR, 1.31; 95% CI, 1.25 to 1.37), iliac artery aneurysms (HR, 1.60; 95% CI, 1.33 to 1.91), and other abdominal aneurysms (HR, 1.58; 95% CI, 1.39 to 1.79). But there was little association with increased incidence of aortic dissection (HR, 1.09; 95% CI, 0.98 to 1.13).
When stratified by age, all adults 35 and older appeared to be at higher risk (18 to 34 years: HR, 0.99; 95% CI, 0.83 to 1.18; 35 to 49 years: HR, 1.18; 95% CI, 1.09 to 1.28; 50 to 64 years: HR, 1.24; 95% CI, 1.19 to 1.28; P = .04). Minimal differences were seen when the cohort was stratified by sex and comorbidities.
"These data collectively suggested that fluoroquinolone use was associated with an increased risk of aneurysm among all adults aged 35 years or older and that other traditional risk factors, such as sex and comorbidities, may also be associated with aneurysm among adults, although the association may be minimal," the authors wrote.
"Contextualizing these data, we believe that the current US FDA black box warnings are warranted but may need to be expanded to include younger adults with other risk factors," they concluded.
That recommendation is echoed by clinicians with the University of Florida College of Medicine, who wrote in an accompanying commentary that the large cohort study "suggests it is time to rethink the use of this class of antibiotics for patients with or without aortic disease."
Fluoroquinolone safety warnings
The 2018 safety warning is one of several that have been issued in recent years by the FDA for fluoroquinolones. These antibiotics—which include drugs such as ciprofloxacin, moxifloxacin, levofloxacin, gemifloxacin and more than 60 generics—cover a broad-spectrum of gram-positive and gram-negative bacteria and are used to treat a variety of common bacterial infections.
In 2008, the agency added a warning that fluoroquinolone use increased the risk of tendinitis and tendon rupture. That was followed by a 2013 label update that warned that fluoroquinolones taken by mouth or by injection may cause peripheral neuropathy, a nerve condition that can cause weakness, numbness, and pain in the hands and feet.
In 2016, the FDA revised the black box warning, advising that fluoroquinolone use was associated with increased risk of disabling and potentially permanent side effects involving tendons, muscles, joints, nerves, and the central nervous system, and that patients who have acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections should use the drugs only if no other options are available.
The authors of the study say further research is needed to clarify the mechanism behind fluoroquinolone-associated aneurysm development.