 A study conducted in England found that nurses are increasingly responsible for antibiotic prescriptions and should be included in antimicrobial stewardship (AMS) efforts, researchers reported late last week in the Journal of Antimicrobial Chemotherapy.
A study conducted in England found that nurses are increasingly responsible for antibiotic prescriptions and should be included in antimicrobial stewardship (AMS) efforts, researchers reported late last week in the Journal of Antimicrobial Chemotherapy.
Using National Health Service antibiotic dispensing data from 2014 through October 2021, researchers from Cardiff University and the University of Reading estimated the proportion of antibiotic prescriptions dispensed in the community by nurse independent prescribers (NIPs) and general practitioners (GPs) over time. They also looked at the impact of COVID-19 on the volume, rate, and type of antibiotic prescriptions dispensed.
More than doubling of antibiotics prescribed by nurses
Over the study period, the number of NIPs in England nearly doubled (from 24,457 to 41,649) and the number antibiotic prescriptions dispensed by NIPs rose by 146% (from 14,225 to 34,997). The proportion of dispensed antibiotics prescribed by NIPs rose from 7.5% in 2014 to 9.6% in 2020. But the rate of dispensed antibiotic prescriptions per prescriber per calendar year decreased by 50% for NIPs and by 21% for GPs from 2014 through 2020, a trend that continued across both groups following the onset of the COVID-19 pandemic.
The five most commonly prescribed antibiotic classes were similar for GPs (penicillins, tetracyclines, macrolides, nitrofurantoin, and suplhanomides/trimethoprim) and NIPs (penicillins, nitrofurantoin, tetracyclines, macrolides, and sulphanomides/trimethoprim).
The study authors note that while NIPs are playing an increasing role in primary care and antibiotic prescribing, their contribution to AMS and potential impact on antimicrobial resistance (AMR) are absent from the United Kingdom's national AMR action plan, which aims to reduce antibiotic use in humans by 15% by 2024.
[Nurse independent prescribers] are an increasing contributory influence on total antibiotic prescribing and an important group to include in [stewardship] efforts.
"NIPs are an increasing contributory influence on total antibiotic prescribing and an important group to include in AMS efforts," they concluded. "NIPs prescribe fewer antibiotics than GPs but work under different conditions, e.g. longer consultations and less complex patients, so interventions should be tailored to this group and the population and context in which they are delivered."
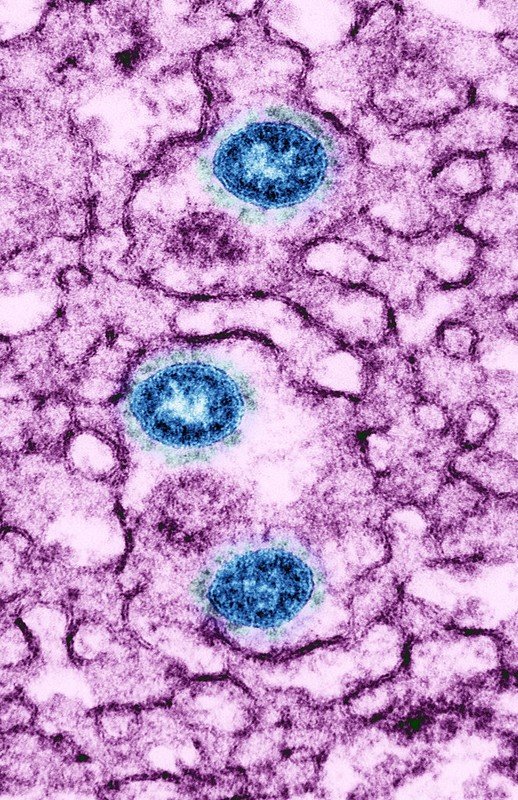
 Infection with the SARS-CoV-2 Omicron variant is less likely to lead to long COVID than previous variants, and prior infection—but not monovalent (one-strain) vaccination—helps protect against persistent symptoms, suggests a
Infection with the SARS-CoV-2 Omicron variant is less likely to lead to long COVID than previous variants, and prior infection—but not monovalent (one-strain) vaccination—helps protect against persistent symptoms, suggests a  A
A 














