The Centers for Disease Control and Prevention (CDC) has identified two independent outbreaks of pan-resistant strains of the deadly yeast Candida auris, according to last week's Morbidity and Mortality Weekly Report (MMWR).
The report described two clusters of pan-resistant C auris identified through routine screening by the CDC’s Antibiotic Resistance Laboratory Network from January through April of this year. The clusters involved three patients at a long-term care facility in Washington, DC, and seven patients in two acute care hospitals in Texas.
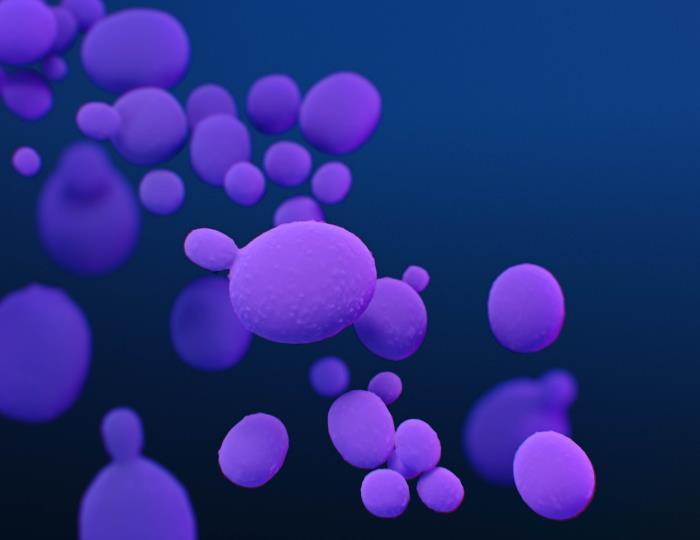
The multidrug-resistant yeast, first identified in Japan in 2009, arrived in the United States in 2016 and has slowly spread in healthcare facilities since its arrival, predominantly among immune-compromised patients in long-term care facilities and acute care hospitals. While many C auris cases have been resistant to azoles and polyenes—two of the three major classes of antifungals used to treat Candida infections—the 10 cases identified in the two clusters were also resistant to echinocandins, which are the first-line treatment for invasive C auris infections.
Pan-resistant C auris cases have been previously identified in US patients, but what sets these cases apart is that the patients had no previous exposure to antifungal treatment. In previous cases, notably three identified in New York City in 2017 and 2018, resistance to echinocandins developed after the patients were treated with the antifungal. In these outbreaks, the pan-resistant strains appear to have originated before treatment and then spread among patients in the facilities.
"We're seeing this in two unrelated situations where this high level of resistance seems to be spreading," said the CDC’s Meghan Lyman, MD, lead author of the report. "That's obviously very concerning, because now it means that any high-risk individual could acquire it and then develop a severe infection that has very limited treatment options."
Infections and colonization
The three pan-resistant cases in Washington, DC, were identified through a skin colonization screening at a long-term care facility for severely ill patients. Of the seven cases in the two Texas facilities—a long-term acute care hospital and a short-term acute care hospital in the same city—four were identified through colonization screening and three had invasive infections.
"Obviously the infections are more severe, and a few of them were bloodstream infections, but even in the colonization cases, we're still concerned about those because they can spread to other people who could develop infections," Lyman said. As prior research has shown, 5% or 10% of colonized patients will likely go on to develop invasive infections.
Overall, susceptibility testing of C auris isolates in the United States has shown that 85% are resistant to azoles, 33% are resistant to the polyene antifungal amphotericin B, and 1% are resistant to echinocandins, according to the report. As a result, echinocandins have become the primary treatment for invasive C auris infections.
"Echinocandins have really been the medications we've relied on for treatment," Lyman said.
Of the 10 cases, five were pan-resistant and five (all in Texas) were resistant to both echinocandins and azoles.
Combined 30-day mortality from both outbreaks was 30%, although whether those deaths were caused by C auris is unclear. Lyman said there was limited information on the effectiveness of treatments.
Containment is a challenge
Resistance isn't the only issue with C auris. The ability of the fungus to spread easily in healthcare settings is another trait that concerns public health officials and infectious disease experts.
Unlike other species of Candida, which tend to colonize the gut, C auris has an affinity for skin, and CDC research has shown that colonized patients can shed the pathogen onto bed rails and other parts of the hospital environment. There, it can survive for several weeks, and it can be hard to kill with standard disinfectants.
In addition, C auris often spreads between facilities within healthcare networks when colonized or infected patients are transferred.
"It makes the containment really challenging, because you can't just focus on one facility," Lyman said. "When you find it in a facility, it may just be the tip of the iceberg, and there are a lot of other cases that may have gone undetected."
While the patients within the two clusters had overlapping healthcare exposures that likely contributed to the outbreaks, no known epidemiological links were identified between them. Lyman said whole-genome sequencing is underway to determine how related the strains are to strains in other geographic areas.
Although the CDC says C auris tracking updates have been delayed because of the COVID-19 pandemic, 948 clinical cases were reported from 19 states from May 1, 2020, to Apr 30, 2021, and screening identified 2,193 colonized patients. Lyman said the pandemic may have contributed to an increase in cases, since some patients with severe COVID-19 have required intubation and other invasive devices that put them at higher risk of C auris infection.
Lyman said the agency is working with local health departments in places where C auris has been identified to prevent spread of the pathogen through early identification and better infection prevention and control practices.