Editor's Note: Part 2 of a two-part commentary. Part 1, published yesterday, outlined the differences in face coverings masks, the science of respiratory protection, and the hierarchy of disease controls.
Dr Brosseau is a national expert on respiratory protection and infectious diseases and a research consultant with the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota (UMN). Dr Ulrich is a UMN assistant professor in the Division of Environmental Health Sciences and a CIDRAP researcher. Dr Escandón is a physician and infectious diseases researcher in the Division of Infectious Diseases and International Medicine at UMN and also collaborates on research with CIDRAP. Cory Anderson is a graduate research assistant with CIDRAP. Dr Osterholm is CIDRAP director and Regents Professor at UMN.
_____________________________________
As noted in part 1, not all facepieces designed to protect against respiratory diseases like COVID-19 are created equal, and they must be considered as only one tier in a hierarchy of protective steps.
Here in part 2 we spell out why not all studies involving cloth face coverings or surgical/medical masks warrant equal consideration. We'll detail the necessary elements of a rigorous study and explore some recent studies that, though highly touted by both scientists and the lay press, fell quite a bit short of the ideal.
Again, at the outset, we underscore that we are not "anti-mask." Rather, we are in favor of wearing the most protective type of facepiece for the setting—such as a non-fit tested respirator when spending more than a few minutes in a crowded, indoor space—and only in combination with other interventions.
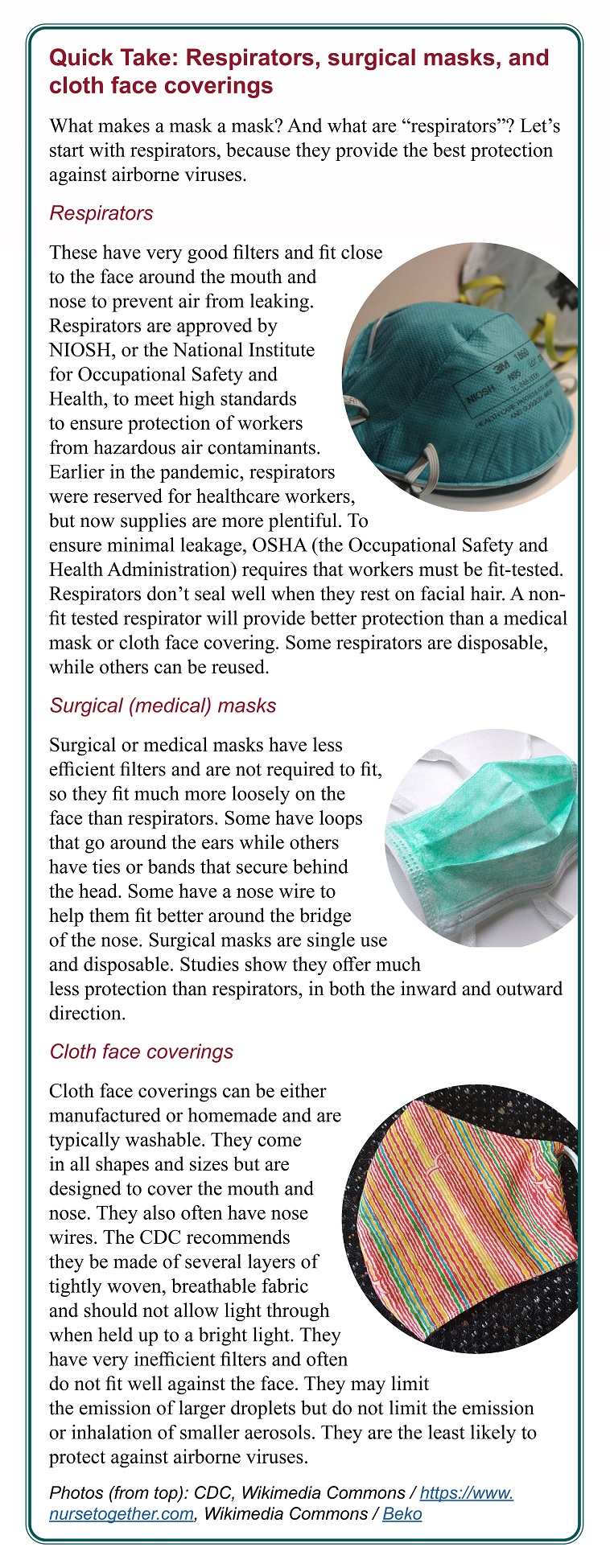 Also, for simplicity, we broadly use "masks" to refer to cloth face coverings as well as surgical masks and "surgical masks" to refer to medical-use masks. Respirators like N95s are not considered to be masks (see sidebar at left).
Also, for simplicity, we broadly use "masks" to refer to cloth face coverings as well as surgical masks and "surgical masks" to refer to medical-use masks. Respirators like N95s are not considered to be masks (see sidebar at left).
Importance of a body of evidence
Not all scientific findings hold equal weight. An important hierarchy of evidence exists in science, which progresses from laboratory studies to real-world clinical or epidemiologic studies.
Laboratory studies of interventions, such as those of masks or ventilation, are an important first step to building a body of evidence for efficacy. The advantages are that important variables can be controlled, well-characterized, and tested for their impact on exposure. Any test of an intervention in the real world should be accompanied by, at a minimum, an assessment of the intervention using standardized laboratory performance tests, to provide context and allow comparisons among studies.
As an example, when a mask or respirator is tested in actual use, data about filter performance, breathing resistance, and fit in a controlled setting on human subjects should also be provided for context and to allow comparison with other studies. Cloth face coverings and surgical masks, in particular, exhibit a wide range of performance in each of these variables; thus, a study of one surgical mask in a community setting cannot be easily equated with a study of another, different surgical mask in a healthcare setting.
Clinical or epidemiologic studies also follow a progression, from case reports to systematic reviews and meta-analyses. Randomized controlled trials (RCTs)—often deemed gold standards—are considered a higher level of evidence than case reports or observational studies, but they are not without weaknesses and limitations. A single RCT is most useful if it is generalizable to and reproducible in other settings. An RCT that fails to account for important difference between its intervention and control arms may offer less quality information than does a well-conducted observational study such as a cohort study or case-control study. Systematic reviews and meta-analyses offer two advantages—they consider a large body of evidence, and they rate the quality of each piece of evidence.
A living rapid review of masks, first published in June 2020 and supported by the Pacific Northwest Evidence-based Practice Center at Oregon Health & Science University, has been updated six times throughout the pandemic. It examined studies comparing face mask effectiveness in community and healthcare settings for SARS-CoV-1 (the virus that causes SARS), SARS-CoV-2, MERS-CoV (which causes MERS), and other viral respiratory diseases, including influenza.1–7 Reviews like this follow a very specific process to evaluate studies' quality.
The original review did not find any data on SARS-CoV-2 but concluded from data on other similar pathogens that the mask effectiveness evidence was strong in healthcare settings, with N95 respirators more effective than surgical masks. The evidence regarding the effectiveness of masks in community (non-healthcare) settings was much weaker.
In the first alert (update), one new community study of cloth face coverings for SARS-CoV-2 offered some evidence of effectiveness, but reviewers concluded that the strength of evidence was insufficient. New studies in alerts 2 through 5 were considered insufficient for evidence of cloth face coverings or surgical mask effectiveness in healthcare settings.
In alert 6, published in July 2021, a cross-sectional healthcare study found that consistent use of surgical masks was associated with a slightly reduced risk of SARS-CoV-2 infection, when compared with inconsistent mask use. In community settings, evidence remained low for any association between face covering or surgical mask use and SARS-CoV-2 infection.
Thus, very little has changed in terms of the team's conclusions about the efficacy of masks in healthcare or community settings throughout the pandemic.
What makes for a good mask study? (and why most fail)
A well-conducted laboratory study of face coverings, masks, or respirators requires the use of standardized and certified performance tests. Filters should be tested with aerosols in the most penetrating particle size (generally around 0.3 micrometers, or microns) at a high flow rate (at least 84 liters per minute) that distinguishes high- from low-performing filters. Air flow resistance (pressure drop) should be measured at the same high flow rate.
At a minimum, inward leakage, using a standardized quantitative method such as described in the US OSHA Respiratory Protection Standard, should be measured on a panel of human subjects, preferably with a range of face sizes.8,9
As noted above, there is not yet a standardized performance test for outward leakage (source control). The methods used by Lindsley et al10 (2021) are perhaps the most appropriate while we wait for scientists to conduct the necessary research.
For any study of masks in real-world settings, the data described above should be assessed and reported, to allow comparison with the wide range of available face coverings, masks, and respirators.
A rigorous, reliable epidemiologic mask study is very difficult to design and conduct. During a pandemic, there are many unknowns, such as how infection occurs, the modes of transmission, and who transmits to whom and when. Later in a pandemic, further challenges arise. It may be difficult to determine who has been infected and who remains uninfected.
Public health guidelines are constantly changing as new knowledge is gained. Multiple interventions occur simultaneously. Populations and locations differ in demographics or other significant ways. With time, a large fraction of the population will be immune, making it more difficult to find naïve (never-infected) subjects. These issues make it challenging to conduct an RCT that allows conclusions to be drawn about cause and effect. Of note, RCTs can hardly capture the complexities related to viral transmission and public health interventions, although cluster-randomized trials attempt to do so. Complex systems methodologies and diverse evidence approaches, including observational and mechanistic evidence, are therefore needed.11–13
Some key elements to consider when evaluating an epidemiologic study of an intervention such as masks include:
- An outcome measure, such as SARS-CoV-2 antibodies, that clearly determines who is infected.
- A way to account for and control for all simultaneous interventions.
- Uniformity in how people wear face coverings, masks, or respirators.
- Consideration of all variables relevant to both SARS-CoV-2 exposure and infection.
- Consistent exposure levels between intervention and control groups.
- Appropriate statistical analysis.
First, the outcome measure—or the variable used to determine if infection was prevented by mask wearing—must clearly discriminate between people who are and are not infected. For COVID-19, one commonly used outcome measure is seropositivity, or detection of SARS-CoV-2 antibodies in the blood. Seropositivity must be measured in every subject as they are enrolled in the study. If subjects are seropositive at baseline, they must be excluded from analyses that consider infection as the outcome; otherwise, their lack of infection during the study period may be incorrectly ascribed to the intervention (e.g., mask) rather than to natural protective immunity from previous infection. Seropositivity must then be measured in every subject during follow-up, not just among those who report symptoms. Otherwise, those with an asymptomatic infection will be incorrectly recoded as uninfected.
Second, all other simultaneous interventions—like mandated closures or physical (social) distancing—must be measured and controlled for to eliminate or greatly reduce confounding. The preference would be, of course, for no other intervention to occur during the study period. Since that is not possible, all interventions should be identified and measured for every subject in all settings where they spend time. The easiest way to account for other interventions is to select groups of people who spend similar amounts of time in similar locations with similar interventions.
If that is not possible, then a thorough and ongoing assessment of each subject's potential location of exposure and time of exposure should be conducted throughout the study. Ideally, this should involve direct observation rather than relying on subjects' self-reports. Such observation involves careful collection of data about the circumstances of every setting in which each subject spends time, including the number of people, type of space, degree of crowding, and type of ventilation, among others. This quickly becomes a complex and difficult task, unless one can identify an easy-to-study population with few differences in their circumstances. For example, recruits sharing barracks for several weeks would be easier to study than members of a community with different jobs and living circumstances.
Third, one must ensure that all interventions are implemented similarly. If the goal is to compare cloth masks with surgical masks, for example, any differences in their performance could be due to their wear time if one mask is more uncomfortable or difficult to wear than the other.
Fourth, analyses must consider other relevant variables that may be associated with both exposure to SARS-CoV-2 and infection. To assess mask wearing for example, analyses should control for relevant demographic variables such as age, ethnicity, and occupation. Job and workplace may also be important, since some types of work are associated with higher infection risks than others. Home location, crowding, types of transport, time spent away from home, and number of household members will all play a role in a subject's exposure level and duration. It is not easy to match on every relevant variable, but it is important to collect as much information about all these variables as possible, so they can be considered during data analysis.
Fifth, exposure matters. If two groups experience different levels of exposure, then an outcome could be due to these differences and not to the intervention itself. For example, if the control group experiences higher exposures due to job, household, or some other variable, a higher rate of seropositivity in the control group would be incorrectly ascribed to the intervention (mask). All variables important to the outcome must be equal at baseline or accounted for throughout the study and included in the data analysis.
Finally, statistical analysis is an extremely important element of any epidemiologic study. Sometimes missing data can be imputed or accounted for, but failure to account for variables at baseline or throughout the study cannot be necessarily fixed later. For example, while matching and randomizing by location, rather than individual, can be a powerful study design, it also requires a more complex analysis that accounts for correlation of subjects within a location.
Studies that fall short of their billing
The studies we highlight here are among the more recent to conclude that masks are highly effective, and they garnered much media attention, sometimes being flagged as studies that finally lay the masking debate to rest.
On closer examination, though, they illustrate our points in the above section about the need for well-conducted studies and highlight the difficulties inherent in evaluating interventions during a pandemic. They represent many of the limitations of similar studies published throughout the pandemic.
While we believe masks have a place in the hierarchy of controls, we urge scientists and journalists to consider their limitations and to focus, instead, on the most effective controls and the combination of multiple interventions to stop or limit SARS-CoV-2 transmission.
Face masks for COVID pass their largest test yet. A rigorous study finds that surgical masks are highly protective, but cloth masks fall short.14
By Lynne Peeples in Nature News, Sep 9, 2021
 A study15 that has received considerable attention in the lay and scientific press compared surgical and cloth masks in a cluster RCT conducted in Bangladesh from December 2020 to January 2021. The study included more than 340,000 adults from 600 communities.
A study15 that has received considerable attention in the lay and scientific press compared surgical and cloth masks in a cluster RCT conducted in Bangladesh from December 2020 to January 2021. The study included more than 340,000 adults from 600 communities.
The intervention communities received free masks, information on the importance of masking, role-modeling by community leaders, and in-person reminders, whereas the control arms did not receive anything. Despite the strengths of this study, including its large sample size and novel study design, it is not yet peer-reviewed. And those who have touted this study in the scientific and popular press have failed to detail its many relevant limitations.
This study took place when considerable infection had already occurred, meaning that subjects may have been seropositive before the study began. Baseline seropositivity rates were not reported for the communities where the study was conducted, although the authors report that "baseline symptomatic seroprevalence" among a random sample of 20% of the baseline blood draws was slightly higher in the control communities compared with intervention communities. Only subjects reporting symptoms during the study were offered testing, and less than half agreed to be tested for seropositivity, meaning that the final number included in the study was much smaller than the 340,000 potential participants.
Because asymptomatic infection is also an important feature of SARS-CoV-2 epidemiology, its measurement should be considered in transmission studies.16 Furthermore, seropositivity based on self-reported symptoms during the study period is not considered a highly reliable measure of infection, especially if seropositivity was not ruled out at baseline. This is because COVID-19 symptoms are not specific and are similar to those of many other respiratory conditions, viral or otherwise.17,18
Second, the study authors provide limited details about the two interventions (cloth masks and surgical masks). They report no data on their filter efficiency, breathing resistance, or fit. Nor do they offer any information on their comfort or how easy they would be to wear over long periods. The surgical masks were washable, which suggests they differ from surgical masks used in US healthcare settings.
Finally, the authors indicate that, after the intervention, symptomatic seroprevalence was higher in control communities (adjusted prevalence ratio [aPR], 0.91; 95% confidence interval [CI], 0.82 to 1.00), and that the relative reduction in risk was greatest in communities randomized to surgical compared to cloth masks or no mask (aPR, 0.89; 95% CI, 0.78 to 1.00). Note, however, that the confidence intervals for both measures were wide—indicating less confidence in the findings—and included 1.0. An aPR of 1.0 indicates that one cannot conclude that the masks provided any protection.
So, while this is the largest study to date of the effectiveness of masks in a community setting, the results must be interpreted within the context of these key study limitations. Also, the study is still a pre-print, meaning it has not yet been peer-reviewed. Many of the issues outlined above should be addressed in any final version published in a peer-reviewed journal. One appropriate interpretation of the results of this study includes the fact that this study offers some evidence that the use of masks in a community setting may offer some, however minimal, protective benefit—which is not nearly as captivating as the headlines this study has earned to date.
We studied one million students. This is what we learned about masking.
New York Times guest essay19 by Kanecia Zimmerman, MD, and Danny Benjamin, Jr, MD, Aug 10, 2021
 In a New York Times essay, Drs Zimmerman and Benjamin describe their study of 1 million students, concluding that universal masking was responsible for low SARS-CoV-2 transmission in schools. They did not provide data to support this claim and did not provide access to a publication, peer-reviewed or otherwise, for readers to assess the data for themselves.
In a New York Times essay, Drs Zimmerman and Benjamin describe their study of 1 million students, concluding that universal masking was responsible for low SARS-CoV-2 transmission in schools. They did not provide data to support this claim and did not provide access to a publication, peer-reviewed or otherwise, for readers to assess the data for themselves.
More than a month later, a peer-reviewed paper by the authors and their colleagues was posted online by Pediatrics.20 The study included a little more than 138,000 students and 23,000 staff in 13 North Carolina school districts, well short of 1 million students. The outcome was school-acquired infections based on contact tracing and confirmed by molecular testing, although the latter was not required, and it is unclear whether reported cases were limited only to those with positive tests.
The authors considered masking as a main intervention of the study, but there was no formal control group, since all schools were in districts with universal masking policies. Daily walkthroughs were performed by school personnel to confirm that everyone was wearing a mask, but no effort was made to check whether masks were used at the time of suspected exposure for school-acquired infections. The weekly infection rates per 100 people were very low (near zero) throughout the study period for older students in secondary schools and ranged from less than 1 to near 4 per 100 people for younger primary school students. The latter were less than weekly community rates but mirrored the weekly community trend throughout the study period.
Infections for staff versus students were not reported separately, which is a serious weakness given the much greater risk of infection among adults than children. As well, staff had much greater exposure time, since they were teaching throughout the week, while students were attending school every other day.
The authors argue that, because there were no improvements in ventilation and physical distancing was typically less than 6 feet, universal masking must be responsible for low infection rates. They recognize some key weaknesses of their study, the most important being that there was no comparison group or a period when masks were not required. Lacking information about rates in students versus staff, whether universal masking was in place for those infected, or any other relevant details about exposure for those in primary school, we believe these authors overstate the significance of their findings.
Rather, we believe that the more important findings of this study are: (1) school sports accounted for 75% of school-acquired infections for high school students and staff, with indoor basketball playing a large role in transmission and (2) minimizing the number of students in a classroom and using a hybrid model with cohorts attending school on alternating dates most likely played an important role in minimizing infection rates.
This peer-reviewed publication and associated guest essay are good examples of how easy it is for investigators to find what they're looking for and derive their conclusions based on their beliefs, rather than on information provided by a very limited dataset.
Masks limited COVID transmission in unvaxxed college kids21
— "Modified quarantine" protocol incorporating mask usage also played a role
by Zaina Hamza, Staff Writer, MedPage Today, Sep 10, 2021
 A study22 published in Morbidity and Mortality Weekly Report (MMWR) compared transmission to contacts of masked and unmasked students from January to May 2021. The individual-level exposure data are more robust than in the North Carolina study described above, with information available on mask wearing and the number of exposures for each positive case and their contacts, as well as confirmation of infection by polymerase chain reaction, a reliable test. Data analyses considered demographics and exposure.
A study22 published in Morbidity and Mortality Weekly Report (MMWR) compared transmission to contacts of masked and unmasked students from January to May 2021. The individual-level exposure data are more robust than in the North Carolina study described above, with information available on mask wearing and the number of exposures for each positive case and their contacts, as well as confirmation of infection by polymerase chain reaction, a reliable test. Data analyses considered demographics and exposure.
There were 378 close contacts of 265 students with positive tests; 26 reported only mask wearing exposure and 352 had some unmasked exposures. Of the 378 close contacts, 31% (116) had positive tests. The positivity rate was 5.4 times higher in those reporting any unmasked exposure (32%) than in those reporting only masked exposures (8%). The investigator also found a statistically significant difference in infection rates by vaccination status, although the numbers of vaccinated students were small (0% infection rate in 18 fully vaccinated, 21% in 24 partially vaccinated, and 33% in 336 unvaccinated). Contacts reporting a median of 2 exposure incidents were more likely to be infected than those with a median of 1 (P < 0.001).
These results illustrate the importance of considering exposure time, especially when exploring the efficacy of masks. Unfortunately, no data were provided about the type of masks typically worn by students. As well, the information about exposure focuses only on the number of interactions over 15 minutes, not the total exposure time. We suspect that exposure time, regardless of mask status, would be a strong predictor of infection.
The MedPage writer adequately describes the study limitations, the most important of which may be that the study was conducted before the Delta variant became the dominant strain in the United States. And while the author does not oversell the efficacy of masks in the text, making clear that both mask wearing and exposure were important variables associated with infection, the title emphasizes only mask wearing as an important variable. Thus, the story in MedPage focused almost exclusively on masking and neglected the important messages about getting vaccinated and minimizing exposure.
A Calif. elementary school teacher took off her mask for a read-aloud. Within days, half her class was positive for delta.23
By Ariana Eunjung Cha, Washington Post, Aug 28, 2021
 This study,24 published on Aug 27, 2021, in MMWR, is one of very few published so far during the recent surge caused by the Delta variant, which is known to be more transmissible in all age-groups. Despite many interventions, including face masks on students and teacher, 6 feet between desks, open doors and windows and a portable air cleaner, an unvaccinated elementary school teacher who was symptomatic for 2 days before testing positive infected 12 students in a single classroom (8 of 10 in the front 2 rows and 4 of 14 in the back 3 rows).
This study,24 published on Aug 27, 2021, in MMWR, is one of very few published so far during the recent surge caused by the Delta variant, which is known to be more transmissible in all age-groups. Despite many interventions, including face masks on students and teacher, 6 feet between desks, open doors and windows and a portable air cleaner, an unvaccinated elementary school teacher who was symptomatic for 2 days before testing positive infected 12 students in a single classroom (8 of 10 in the front 2 rows and 4 of 14 in the back 3 rows).
The teacher apparently removed his or her mask to periodically read out loud. (The article does not mention the gender of the teacher; the journalist assumed the teacher was female.) Also, the MMWR report does not specify how much the teacher moved around in the classroom and how long the mask was off.
It is difficult to conclude that masks were effective at preventing transmission, given the very high attack rates in the classroom when all students were supposedly wearing masks. It is very likely that, even if the teacher had worn a mask for the entire classroom time, the same number of students would have been infected, because the exposure time involved days, not hours.
The attack rate was highest for students in the front row and lowest for those in the back row. If desks were 6 feet apart, the two infected students in the last row were more than 24 feet from the infected teacher. These results suggest that air flowed from the front to the back of the room and that particles were diluted as they traveled from the source—the infected teacher. Thus, physical distancing was only partially successful at limiting students' exposures, again highlighting the importance of exposure time.
The open windows and portable air cleaner may not have been deployed effectively to remove infectious particles from the space. It may be that the windows did not establish an effective cross draft and the air cleaner may have caused air movement toward the back of the room. An air cleaner cannot effectively remove particles if it is not located very close to the infectious source.
Children in other classrooms and children and parents in households and parties away from school were also infected, highlighting the problem with relying on masks in only some settings (classrooms) and not in others (households). Every exposure has the potential to lead to an infection.
In their discussion, the authors of this study do not oversell the efficacy of masks, nor do they blame the teacher for failing to always wear a mask. Rather, their primary messages are the importance of vaccination and the use of multiple interventions, including ventilation, masking, testing, and staying home when symptomatic.
The infographic accompanying this study, however, appears to lay the blame for infection on the teacher's failure to wear a mask continuously and overemphasizes the effectiveness of masks in preventing transmission. And the Washington Post and other news outlets focused on the message about masks illustrated in the infographic, blaming the teacher for exposing students by removing his or her mask when reading out loud. The headline fails to appropriately communicate the nuances of this scenario.
The importance of peer review and accurate messaging
Science has never been more at the forefront of public discussion and scrutiny than during the COVID-19 crisis. The most important role scientists play during a pandemic is to provide the highest quality scientific evidence—and its accurate and fair interpretation—so policymakers can determine how best to protect public health by implementing sound policies.
High-quality science takes time and cannot happen in a vacuum. Peer review—the evaluation of scientific studies by well-qualified experts before publication in journals—has a central role in advancing science, although its value is often unappreciated in both academic and lay scenarios. It is essential that reviewers have both expertise and experience, do not have financial or other conflicts, and understand their role in recognizing strengths and limitations of studies.
Peer reviewers determine if the existing literature is properly acknowledged, methodology of the study is sound, results are interpreted correctly, and conclusions are warranted. Although peer review is a complex and imperfect task that involves human judgment,25 it should always lead to a better product when it involves well-selected subject matter experts.
Unfortunately, the urgency to tackle the pandemic has resulted in early sharing of results, circumventing the important process of peer review. Preprints—articles posted online before peer review and formal publication—have allowed the rapid dissemination of potentially important research with opportunities for open review from more scientists. The negative consequences of unrefereed articles, however, have been significant, including mistrust and misinformation that are difficult to correct later.26
Scientists who skip peer review but fail to convey appropriate context and nuance to their study results can often do more harm than good—as can journalists reporting the results without the proper caveats. Preprints, retractions, and the surrounding controversies are stark reminders that misleading COVID-19 literature challenges the integrity of the scientific process.
Mask wearing has been an extremely polarizing and politicized topic across the world, but especially in the United States.27,28 Endless unrealistic expectations, along with gross misinterpretation and overconfidence, have been evident, including claims that masks alone would "flatten the curve," "end the pandemic," or "reduce the clinical severity of COVID-19."16,29–31 Now, one and a half years into the pandemic, if masks were as effective as many believed them to be, we should have seen significant impacts. But that has not been the case anywhere on the globe.
This is not to say that masks do not play a role in disease control, but that public health officials should not oversell the role of masks. Rather, they need to encourage appropriate mask use in the context of other highly effective interventions such as vaccination.
This far into the pandemic, all mask studies should wait for peer review to help improve the final product. Whether results show that masks are highly effective or not, we should question whether all possible limitations of design, measures, and analyses have been considered.
It is well known that masks and face coverings are highly variable in performance and rarely worn correctly during all possible exposures. Have the authors asked the right questions about other variables that might also explain their results? Were all other interventions accounted for? Is the control group truly a control group (i.e., did the control group subjects also wear masks)? Has the baseline value of the outcome measure been evaluated? Is the outcome measure reliable and valid?
Scientific rigor and accurate communication are a must, no matter the circumstances.25 We cannot expect journalists to ask all these questions or laypeople to understand all the science of masks, but we do expect them to be wary of any study that has not been through the peer review process. In the end, COVID-19 must serve as a catalyst to develop strategies that mitigate the disruption of high-quality research processes, scrutinize papers and correct errors, support open-data policies, and allow a timely response to societal needs.32 A global research perspective is needed in which the highest standards of study planning, data collection, and research reporting are continuously promoted.
It's time to get real (scientific) about masks
It is time to lower the unrealistic expectations about masks—or any single intervention. Public health messaging needs to be focused on many interventions, starting with those at the top of the hierarchy. Masks offer very limited source control and personal protection and should not be considered a replacement for vaccination or equivalent to interventions such as limiting time and the number of people in a shared space or improving air movement.
Scientists must return to the time-honored practice of waiting for peer review before touting their study findings. No single study, regardless of the number of subjects, deserves to skip that important step in the process of building a body of evidence.
We urge journalists to not be taken in by scientists' claims for their non–peer-reviewed studies, even if those scientists hail from highly reputable institutions. Rather, we urge journalists and news outlets to question closely why scientists find it necessary to advertise their study ahead of peer review.
We are well past the emergency phase of this pandemic, and it should be well-known by now that wearing cloth face coverings or surgical masks, universal or otherwise, has a very minor role to play in preventing person-to-person transmission. It is time to stop overselling their efficacy and unrealistic expectations about their ability to end the pandemic.
References
- Chou R, Dana T, Jungbauer R, et al. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2020 Oct 6;173(7):542-55
- Chou R, Dana T, Jungbauer R, et al. Update alert: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2020 Sep 1;173(5):W86
- Chou R, Dana T, Jungbauer R, et al. Update alert 2: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2020 Oct 6;173(7):132
- Chou R, Dana T, Jungbauer R, et al. Update alert 3: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2020 Dec 15;173(12):169
- Chou R, Dana T, Jungbauer R, et al. Update alert 4: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2021 Feb;174(2):W24
- Chou R, Dana T, Jungbauer R, et al. Update alert 5: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2021 Apr;174(4):W47
- Chou R, Dana T, Jungbauer R. Update alert 6: Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med 2021 Sep;174(9):W68
- ASTM. ASTM F3407 - 20. Standard test method for respirator fit capability for negative-pressure half-facepiece particulate respirators. Available from: https://www.astm.org/Standards/F3407.htm
- Zhuang Z, Bradtmiller B, Shaffer RE. New respirator fit test panels representing the current U.S. civilian work force. J Occup Environ Hyg 2007 Jul 23;4(9):647-59
- Lindsley WG, Blachere FM, Beezhold DH, et al. A comparison of performance metrics for cloth masks as source control devices for simulated cough and exhalation aerosols. Aerosol Sci Technol 2021 Oct 3;55(10):1125-42
- Greenhalgh T. Will COVID-19 be evidence-based medicine's nemesis? PLOS Med 2020 Jun 30;17(6):e1003266
- Victora CG, Habicht J-P, Bryce J. Evidence-based public health: moving beyond randomized trials. Am J Public Health 2004 Mar;94(3):400-5
- Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet 2017 Dec;390(10112):2602-4
- Peeples L. Face masks for COVID pass their largest test yet. Nature 2021 Sep 9
- Abaluck J, Kwong LH, Styczynski A, et al. The impact of community masking on COVID-19: a cluster-randomized trial in Bangladesh. Preprint at poverty-action.org. 2021. Available from: https://www.poverty-action.org/publication/impact-community-masking-covid-19-cluster-randomized-trial-bangladesh
- Escandón K, Ulrich AK, Chou R. Concerns with and recommendations for COVID-19 research related to asymptomatic infection and mask wearing. Clin Infect Dis Mar 2021 (published online Mar 23)
- Grant MC, Geoghegan L, Arbyn M, et al. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): a systematic review and meta-analysis of 148 studies from 9 countries. PLOS One 2020 Jun 23;15(6):e0234765
- Jutzeler CR, Bourguignon L, Weis CV, et al. Comorbidities, clinical signs and symptoms, laboratory findings, imaging features, treatment strategies, and outcomes in adult and pediatric patients with COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020 Sep;37:101825
- Zimmerman K, Benjamin Jr D. We studied one million students. This is what we learned about masking. 10 Aug 2021. New York Times. Available from: https://www.nytimes.com/2021/08/10/opinion/covid-schools-masks.html
- Zimmerman KO, Brookhart MA, Kalu IC, et al. Community SARS-CoV-2 surge and within-school transmission. Pediatrics 2021 Jul 28;148(4):e2021052686
- Hamza Z. Masks limited COVID transmission in unvaxxed college kids. 10 Sep 2021. MedPage Today. Available from: https://www.medpagetoday.com/infectiousdisease/covid19/94464
- Rebmann T, Loux TM, Arnold LD, et al. SARS-CoV-2 transmission to masked and unmasked close contacts of university students with COVID-19—St. Louis, Missouri, January–May 2021. MMWR Morb Mortal Wkly Rep. 2021 Sep 10;70(36):1245-8
- Cha AE. A Calif. elementary school teacher took off her mask for a read-aloud. Within days, half her class was positive for delta. 28 Aug 2021. Washington Post. Available from: https://www.washingtonpost.com/health/2021/08/28/delta-variant-unvaccinated-children-elementary-schools/
- Lam-Hine T, McCurdy SA, Santora L, D, et al. Outbreak associated with SARS-CoV-2 B.1.617.2 (Delta) variant in an elementary school—Marin County, California, May–June 2021. MMWR Morb Mortal Wkly Rep. 2021 Sep 3;70(35):1214-9
- Orellana-Serradell O, Díaz MC, González MF, et al. Does peer reviewing for COVID-19-related papers still work? Front Res Metrics Anal 2020 Oct 8;5:571886
- Escandón K, Rasmussen AL, Bogoch II, et al. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infect Dis 2021 Dec 27;21(1):710
- Lee C, Yang T, Inchoco GD, et al. Viral visualizations: How coronavirus skeptics use orthodox data practices to promote unorthodox science online. Proc 2021 CHI Conf Hum Factors Comput Syst. 2021 May 6;:1-18
- Lang J, Erickson WW, Jing-Schmidt Z. #MaskOn! #MaskOff! Digital polarization of mask-wearing in the United States during COVID-19. PLOS One. 2021 Apr 28;16(4):e0250817
- Rasmussen AL, Escandón K, Popescu SV. Facial masking for Covid-19. N Engl J Med 2020 Nov 19;383(21):2092
- Brosseau LM, Roy CJ, Osterholm MT. Facial masking for Covid-19. N Engl J Med 2020 Oct 19;383(21):2092-3
- Escandón K, Martin GP, Kuppalli K, et al. Appropriate usage of face masks to prevent SARS-CoV-2: Sharpening the messaging amid the COVID-19 pandemic. Disaster Med Public Health Prep 2020 (published online Sep 10)
- Horbach SPJM. No time for that now! Qualitative changes in manuscript peer review during the Covid-19 pandemic. Res Eval 2021 Jan 5























