- The US Centers for Disease Control and Prevention (CDC) today released consolidated, evidence-based guidance for preventing the spread of a host of infections in primary and secondary schools. It covers steps schools can take to curb the spread of both respiratory and stomach viruses, as well as bacterial illnesses such as strep throat. In a press release, the CDC said the goal is to maximize school attendance, and the agency said it is releasing the guidance now so that schools can use it to prepare for the 2024-25 school year. Some of the steps include reinforcing proper hand hygiene and respiratory etiquette, improving building ventilation, cleaning and sanitation when appropriate, and promoting vaccination. During outbreaks, the CDC advises schools to take a layered approach, which might include wearing masks and distancing, and screening for illnesses.
- Respiratory illness activity in the United States remained low last week, with no jurisdictions reporting moderate, high, or very high levels, the CDC said today in its weekly respiratory illness snapshot, which covers COVID-19, seasonal flu, and respiratory syncytial virus (RSV). Flu test positivity declined last week, and COVID and RSV test positivity remained stable compared to the previous week. For COVID, wastewater detections of SARS-CoV-2 remained at the minimal level. And for influenza A, which the CDC is now tracking to support H5N1 avian flu monitoring, wastewater detections over the most recent 2 weeks were in the high category at four sites: two in California (San Francisco/San Mateo and Sonoma), and one each in Kansas (Saline County) and Texas (Dallas). The CDC received reports of 3 more pediatric flu deaths, raising the season's total to 167.
- Three countries reported more polio cases this week, including Afghanistan, which reported its third wild poliovirus type1 (WPV1) case of the year, according to the latest weekly update from the Global Polio Eradication Initiative. Two countries reported cases involving circulating vaccine-derived poliovirus type 2 (cVDPB2). Nigeria reported 5 cases, which bring its total for the year to 17. Yemen reported 2 new cases, and 7 for the year.
Quick takes: School infection prevention, low US respiratory virus levels, polio in 3 nations
Study examines impact of azithromycin given during labor
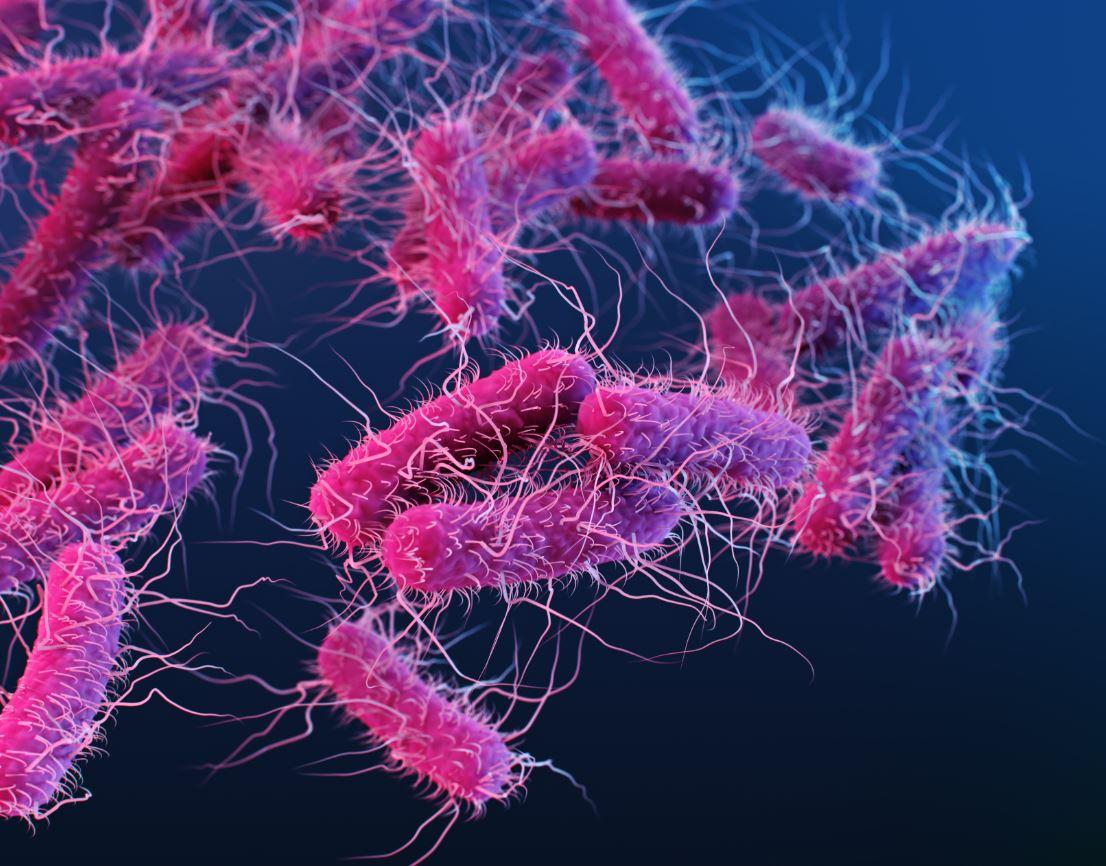
A sub-study of a randomized trial conducted in two African countries found that azithromycin administration during childbirth reduced Escherichia coli prevalence in infants but increased Klebsiella pneumoniae carriage and azithromycin resistance in both bacteria, researchers reported yesterday in Clinical Infectious Diseases.
The phase 3 PregnAnZI-2 trial recruited and randomized 12,000 women in Gambia and Burkina Faso to received either oral azithromycin or placebo during labor. Although that trial found that intrapartum azithromycin did not achieve the primary outcome of reducing neonatal sepsis and mortality, it did reduce neonatal and maternal infections.
In the sub-study, investigators analyzed breast milk and rectal, recto-vaginal, and nasopharyngeal swab samples from 500 mother-infant pairs recruited for the trial to determine the impact of intrapartum azithromycin on the prevalence of carriage and antibiotic resistance of E coli and K pneumoniae.
Impact observed in infants
While little impact was found on the samples collected from the mothers, E coli carriage in infant rectal samples was lower in the intervention than placebo arm at days 6 (63.0% vs 75.2%; prevalence ratio [PR], 0.84; 95% confidence interval [CI], 0.75 to 0.95) and 28 (52.7% vs 70.4%; PR, 0.75; 95% CI, 0.64 to 0.87) postintervention. But the prevalence of azithromycin-resistant E coli was higher in the azithromycin arm at days 6 (13.4% vs 3.6%; PR, 3.75; 95% CI, 1.83 to 7.69) and 28 (16.4% vs 9.6%; PR, 1.71; 95% CI, 1.05 to 2.79).
For K pneumoniae, carriage in infant rectal samples was higher in the intervention than placebo arm at days 6 (49.6% vs 37.2%; PR, 1.33; 95% CI, 1.08 to 1.64) and 28 (53.6% vs 32.9%; PR, 1.63; 95% CI, 1.31 to 2.03), and the prevalence of azithromycin-resistant K pneumoniae was higher in the azithromycin arm at day 28 (7.3% vs 2.1%; PR, 3.49; 95% CI, 1.30 to 9.37).
The investigators say increased carriage of azithromycin-resistant E coli and K pneumoniae could contribute to the spread of azithromycin resistance in the community.
"These results need to be considered when evaluating the overall impact of the use of azithromycin to prevent maternal, neonatal, or infant infections," they wrote.
ECDC warns of invasive meningococcal infections in travelers from Saudi Arabia
The European Centre for Disease Prevention and Control (ECDC) said today that it is monitoring reports from three countries of invasive meningococcal disease linked to Saudi Arabia travel.
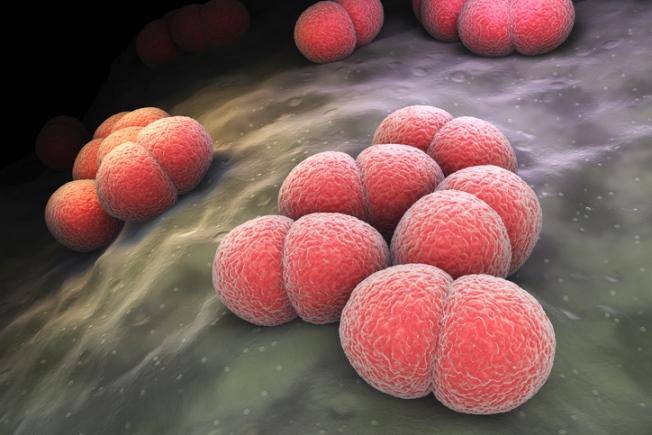
Nearly all cases are in patients who performed the Umrah pilgrimage while in Saudi Arabia, and most cases belong to serogroup W and involve no history of meningococcus vaccination, the ECDC said in a statement.
Invasive meningococcal disease can be severe and has a high fatality rate. Symptoms can include sepsis and meningitis and can progress rapidly without medical support and prompt antibiotic treatment. The infections are most common in young children, adolescents, and young adults.
So far, 12 cases have been reported in France (4), the United Kingdom (3), and the United States (5). Genetic sequencing suggests that some of the cases form a very tight subcluster, which supports an epidemiologic link.
The ECDC said the risk is low for the general public and pilgrims to the Umrah and Hajj who are vaccinated against meningococcal disease. It added that the risk is moderate for unvaccinated pilgrims.
Chicago reports rise in cases, but no common exposures
Separately, the Chicago Department of Public Health this week said it is monitoring an increase in invasive meningococcal disease cases since January 2023. The city typically averages 1 to 3 cases a year, but recorded 7 in 2023 and 8 so far for 2024. Of this year's patients, all had bloodstream infections, and 4 people died.
So far, no common exposures have been identified among the cases. The health department urged city residents to be vigilant for symptoms and to ensure that adolescents are vaccinated and to talk to their healthcare providers about meningococcal vaccines.
The CDPH said Chicago's cases are similar to national trends. In late March, the US Centers for Disease Control and Prevention (CDC) issued a health advisory about a rise in cases, mainly due to Neisseria meningitidis serogroup Y.
Study: Kids with long COVID have impaired exercise capacity
Researchers conducting a small study in Rome discover that, compared with healthy controls, children with long COVID (LC) have objective impaired functional capacity as expressed by a low VO2 peak (oxygen uptake at peak of exercise) during exertion testing.
Kids with LC also showed signs of deconditioning, and cardiogenic inefficiency. The study is published in The Pediatric Infectious Disease Journal.
The study compared 61 children with LC and 29 healthy controls ages 12 and 15. The study authors defined LC as one or more unexplained symptoms for at least 8 weeks after initial infection that negatively impacted daily life. LC is more prevalent in adults than children, but the authors wanted to use cardiopulmonary exercise testing (CPET) to test the health of cardiovascular and ventilatory systems in patients 18 years and younger.
90% of long-COVID patients had health issues
They found that 90.2% of LC patients (55 of 61) had a pathologic test, compared to 10.3% of healthy controls (3 of 29). The mean VO2 peak was 30.17 (±6.85) in LC and 34.37 (±6.55) in healthy patients.
Notably, 48% of the LC patients also had a suspicious phenotype for pulmonary hypertension, the authors wrote.
Our study opens a new scenario in terms of diagnostic possibilities for children
"Our study opens a new scenario in terms of diagnostic possibilities for children with suspected LC, but also a new hypothesis in terms of mechanisms leading to common symptoms in LC, like fatigue and exercise intolerance, suggesting that pediatric LC is a real disease and not a psychologic consequence of the pandemic," the authors concluded.
Global meta-analysis estimates 43% rate of multidrug resistance in COVID patients
A meta-analysis of 173 studies involving nearly 900,000 COVID-19 patients in more than 50 countries finds that 42.9% were infected with multidrug-resistant organisms (MDROs), which the authors say underscores the urgent need for stronger antimicrobial stewardship strategies.
The study, led by Sun Yat-sen University researchers in China, was published in the Journal of Infection.
The investigators systematically reviewed studies published from December 2019 to May 2023 on the prevalence of antimicrobial resistance (AMR) and antibiotic use among COVID-19 patients.
Antibiotic resistance was categorized according to the World Health Organization (WHO) priority list, and antibiotics were classified according to the WHO's Access, Watch, or Reserve (AWaRe) system.
76% of patients were prescribed antibiotics
Of the 892,312 patients, 42.9% had an MDRO infection, with 41.0% testing positive for carbapenem-resistant pathogens, 19.9% for methicillin-resistant Staphylococcus aureus (MRSA), 24.9% for extended-spectrum beta-lactamase (ESBL)-producing organisms, and 22.9% for vancomycin-resistant Enterococcus (VRE) species.
These findings serve as a crucial warning to policymakers, highlighting the urgent need to enhance antimicrobial stewardship strategies to mitigate the risks associated with future pandemics."
A total of 76.2% of patients were prescribed antibiotics, 29.6% with Watch antibiotics, 22.4% with Reserve antibiotics, and 16.5% with Access drugs.
Macrolides were the most commonly prescribed category of antibiotics (34.7%), followed by glycopeptides (33.1%) and third-generation cephalosporins (31.5%). The most commonly used antibiotics were azithromycin (46.2%), ceftriaxone (38.3%), and vancomycin (34.7%).
MDRO prevalence and antibiotic use were significantly greater in low- and middle-income countries than in wealthier countries, with the lowest proportion of antibiotic use (60.1%) and MDRO prevalence (29.1%) in North America. The highest MDRO prevalence was in the Middle East and Africa (63.9%), and the greatest proportion of antibiotic use was in South Asia (92.7%). Antibiotic use and intensive care unit admission were significant predictors of higher MDRO prevalence.
The results underscore "the formidable challenge facing global efforts to prevent and control AMR amidst the backdrop of the COVID-19 pandemic," the researchers wrote. "These findings serve as a crucial warning to policymakers, highlighting the urgent need to enhance antimicrobial stewardship strategies to mitigate the risks associated with future pandemics."











