The antiviral drug remdesivir had little effect in patients with moderate COVID-19 in 105 hospitals in the United States, Europe, and Asia in a randomized, controlled, open-label trial published late last week in JAMA, adding to a mixed picture of the drug in randomized clinical trials (RCTs), which are considered the gold standard for gauging interventions.
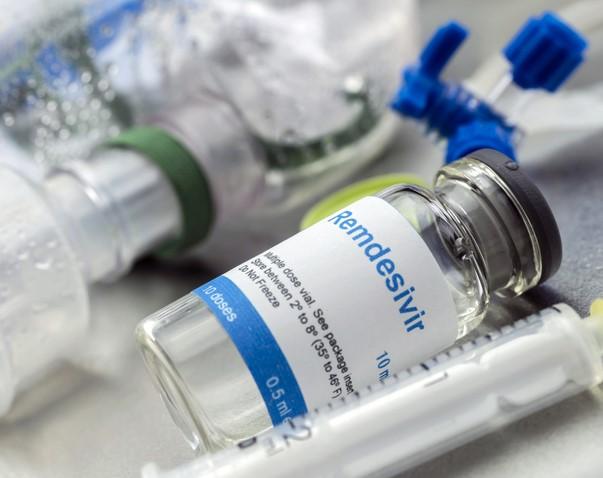
Researchers compared the clinical status of 533 coronavirus patients who had moderate pneumonia and were randomly assigned to receive remdesivir for 5 or 10 days or standard care from Mar 15 to Apr 18. Remdesivir was given in a 200-milligram (mg) intravenous dose on the first day, followed by 100 mg a day.
After 11 days of treatment, patients in the group receiving remdesivir for 5 days had significantly higher odds of clinical improvement on a 7-point ordinal scale than those in the standard-care group (odds ratio [OR], 1.65; 95% confidence interval [CI], 1.09 to 2.48; P = 0.02). But clinical status was not significantly different between the 10-day remdesivir group and the standard-care group (P = 0.18).
Kaplan-Meier estimates of death from any cause at 28 days of treatment were 1% (95% CI, 0.0% to 2.6%) in the 5-day remdesivir group (log-rank P = 0.43 vs standard care), 2% (95% CI, 0.0% to 3.6%) in the 10-day remdesivir group (log-rank P = 0.72 vs standard care), and 2% (95% CI, 0.1% to 4.1%) in the group receiving standard care.
Adverse events, clinical outcomes
Any differences between the groups receiving remdesivir versus standard care in duration of supplemental oxygen or hospitalization were not significant.
Adverse events occurred in 51% of patients in the 5-day remdesivir group, 59% in the 10-day remdesivir group, and 47% in the standard-care group. Nausea was more common in the groups receiving remdesivir than in those receiving standard care (10% vs 3%), as were low blood potassium levels (6% vs 2%) and headache (5% vs 3%).
Nine patients had died by day 28, including 4 in the standard-care group, 3 in the 10-day remdesivir group, and 2 in the 5-day remdesivir group. All deaths occurred in patients 64 and older, and none were attributed to remdesivir therapy.
Median patient age was 57 years, 39% were women, 56% had cardiovascular disease, 42% had high blood pressure, 40% had diabetes, and 14% had asthma. Median length of remdesivir therapy was 5 days for patients in the 5-day group and 6 days for those in the 10-day group. (Patients who improved enough to be released from the hospital didn't finish their treatment course.)
"Among patients with moderate COVID-19, those randomized to a 10-day course of remdesivir did not have a statistically significant difference in clinical status compared with standard care at 11 days after initiation of treatment," the authors wrote. "Patients randomized to a 5-day course of remdesivir had a statistically significant difference in clinical status compared with standard care, but the difference was of uncertain clinical importance."
Perplexingly different study outcomes
Manufactured by Gilead Sciences, remdesivir was granted Emergency Use Authorization by the US Food and Drug Administration for patients 12 years and older with severe COVID-19 on May 20.
Two RCTs at that time had compared clinical benefit of a 10-day course of remdesivir with a placebo. The first trial, conducted in Wuhan, China, didn't find a benefit but had enrolled only 237 patients and may have been underpowered.
The second, a US National Institutes of Health study involving 1,063 patients found that patients given remdesivir for 10 days recovered 4 days sooner than those given a placebo, but there was no significant difference in death rate between those who received remdesivir (7.1%) or placebo (11.9%) (hazard ratio, 0.70; 95% CI, 0.47 to 1.04). The current JAMA study was a continuation of that trial.
In a JAMA commentary that accompanied the current study, Erin McCreary, PharmD, and Derek Angus, MD, MPH, of the University of Pittsburgh School of Medicine said that the different results of the three RCTs could be partially attributed to study design. They added that future studies should address which patients could benefit the most from remdesivir, how long they should receive it, how they will benefit, and what the relative benefit is in patients who also receive dexamethasone or other corticosteroids.
"Some of the RCT findings suggest remdesivir could improve recovery for many millions of individuals around the world who may be hospitalized with COVID-19," McCreary and Angus wrote. "However, the costs to produce and distribute remdesivir at such scale are considerable, and, most importantly, whether remdesivir offers incremental benefit over corticosteroids, which are widely available and inexpensive, is unknown."
Small study of severe COVID shows promise
In contrast with the JAMA study, the Journal of Antimicrobial Chemotherapy yesterday published a small retrospective, observational study in Italy that found that remdesivir may have benefitted COVID-19 patients receiving mechanical ventilation.
Of 51 COVID-19 patients receiving mechanical ventilation at Pesaro hospital from Feb 29 and Mar 20, 25 received 200 mg of intravenous remdesivir for compassionate use on the first day, followed by 100 mg daily on days 2 to 10. Most patients also received other investigational treatments for the coronavirus, such as hydroxychloroquine (64.7%), lopinavir/ritonavir (56.9%), and tocilizumab (17.6%). Twenty-five patients also required dialysis.
The antiviral drug was associated with improved survival (OR, 3.51; 95% CI, 1.77 to 6.95; P < 0.001), and Kaplan-Meier curves demonstrated significantly lower death rates in patients who received remdesivir (56% vs 92%; P < 0.001).
The most common underlying conditions were high blood pressure (54.9%), diabetes (13.7%), ischemic heart disease (13.7%), and moderate kidney failure (7.8%).
Twenty patients completed 10 days of remdesivir treatment, and five (20%) died of COVID-19 infection at a median of 5 days after starting therapy. At final follow-up, 38 patients (74.5%) had died, 9 (17.6%) had been released from the hospital, and 4 (7.8%) remained hospitalized but no longer needed mechanical ventilation.
The authors noted that the study period came at the beginning of the pandemic, when the demand for intensive care unit resources such as ventilators, doctors, and specialized nurses far outstripped the supply, so many patient needs went unmet.
"In conclusion, in this study the mortality rate of patients with COVID-19 under mechanical ventilation is confirmed to be high," they wrote. "The use of remdesivir was associated with a significant beneficial effect on survival."
Observational studies like this one are less valuable than RCTs in assessing a drug and, in fact—as opposed to RCTs—cannot prove that remdesivir actually was the cause of the improved results.