The COVID-19 International Research Team (COV-IRT) and the Children's Hospital of Philadelphia (CHOP) report that they have identified abnormal mitochondrial function in the heart, kidneys, and liver after SARS-CoV-2 infection, which leads to long-term damage and may help explain long COVID.
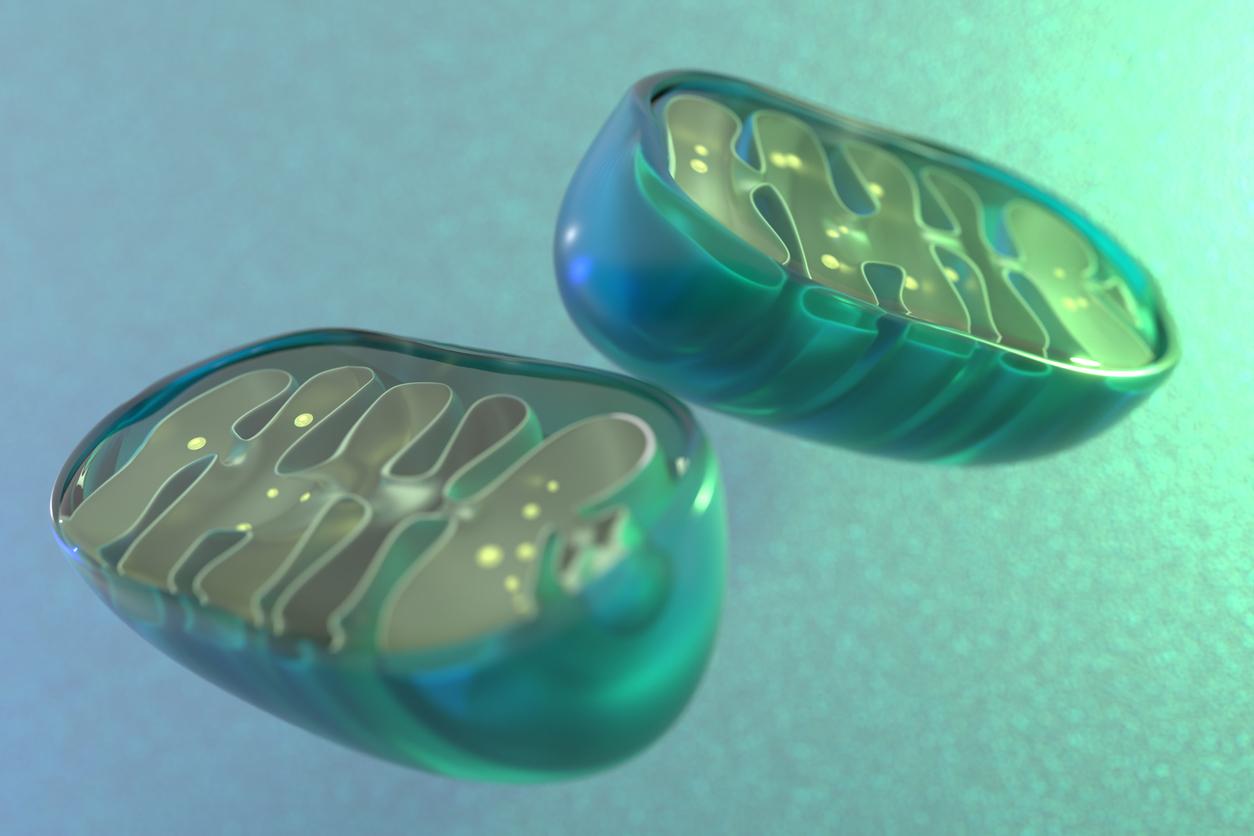
Mitochondria are the so-called "powerhouses" of cells, and the researchers noted that previous studies have shown that SARS-CoV-2 proteins can bind to mitochondrial proteins in host cells, possibly leading to dysregulation.
The team analyzed mitochondrial gene expression in tissues from COVID-19 patients' nose and throat, along with tissues from deceased patients and hamsters and mice. The results were published today in Science Translational Medicine.
"The tissue samples from human patients allowed us to look at how mitochondrial gene expression was affected at the onset and end of disease progression, while animal models allowed us to fill in the blanks and look at the progression of gene expression differences over time," first author Joseph Guarnieri, PhD, a postdoctoral research at CHOP, said in a hospital news release.