COVID-19 infection—even mild cases—can cause substantial long-term changes in the immune system that may be implicated in long COVID, concludes a new observational study by Medical University of Vienna (MUV) researchers published in Allergy.
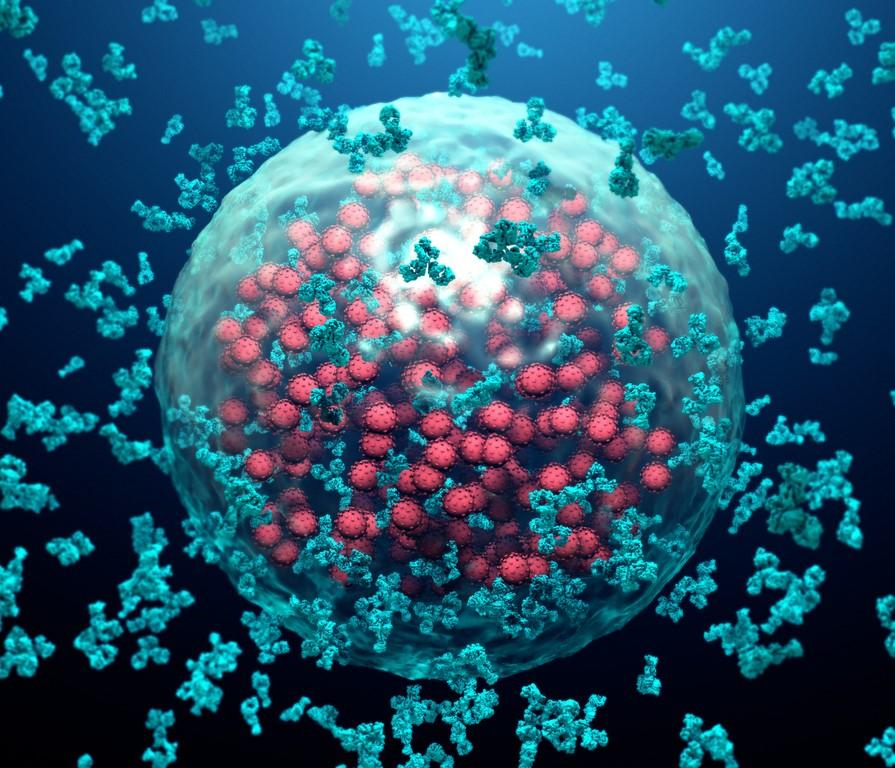
The researchers assessed the number and composition of cellular and humoral immune parameters in the blood (immune cells, cytokines, and growth factors) in 106 COVID-19 survivors 10 months after infection from May to August 2020, a period dominated by the wild-type virus. The team also measured levels of antibodies against the SARS-CoV-2 spike protein (S), receptor-binding domain (RBD), and nucleocapsid protein.
The results were compared with those of 98 matched uninfected people. All participants were unvaccinated because COVID-19 vaccines weren't yet available, and the COVID-19 group wasn't reinfected between study enrollment and the end of the 10-month follow-up.
The team had previously studied the effects of COVID-19 on the immune system in the same cohort 10 weeks post-infection, finding protracted effects even in patients with mild disease. "Not entirely unexpectedly, ten weeks after the infection, the convalescent patients showed clear signs of immune activation of both their T and B cells, in contrast to healthy study subjects," senior author Winfried Pickl, MD, of MUV, said in a university news release.
Drop in immune cells, SARS-CoV-2 antibodies
Cytokines and growth factors in the blood were characteristic of remnants of acute inflammation at 10 weeks post-infection, and a comparison with the patient samples collected 10 months after showed a significant reduction in immune cells, a drop in SARS-CoV-2 antibodies, and a change in growth-factor patterns.
Rather than activation and expansion of certain effector memory cells, transitional B cells, and immature B cells called plasmablasts, the researchers found a significant reduction of adaptive immune cells, including T cells and B cells, at 10 months.
COVID-19 survivors also had significantly upregulated serum interleukin-4 (IL-4) levels and moderately upregulated IL-5 concentrations. Interferon-gamma levels, which were similar to those in the literature for controls and COVID-19 survivors at 10 weeks, had significantly declined by 10 months.
S- and RBD-specific immunoglobulin G antibodies were undetectable in nearly 18% and in more than 80% of the COVID-19 cohort, respectively, by 10 weeks and 10 months. "Moreover, more than 90% of patients lacked neutralizing antibody activity at 10 [months], implying that a large proportion of study subjects after their first infection lost protection from reinfection," the researchers wrote.
A damaged cellular immune system
The authors said the findings may indicate that survivors' immune systems aren't adequately responding to pathogens and may explain some long-COVID signs and symptoms. Long COVID, they added, is presumably caused by long-term impairment in the function of bone marrow, the main producer of immune cells.
Our results provide a possible explanation that certain manifestations of long-COVID-19 may be associated with damage of the cellular immune system by SARS-CoV-2.
"Our results provide a possible explanation that certain manifestations of long-COVID-19 may be associated with damage of the cellular immune system by SARS-CoV-2," they concluded. "This hypothesis can now be investigated in appropriate study populations in detail in the future, and this may contribute to the understanding of pathomechanisms underlying long-COVID-19."