Earlier this week in JAMA, researchers published data on the risk of stroke among Medicare beneficiaries aged 65 years and older in the immediate weeks following a bivalent (two-strain) COVID-19 vaccine dose, finding no significantly elevated risk during the first 6 weeks following injection.
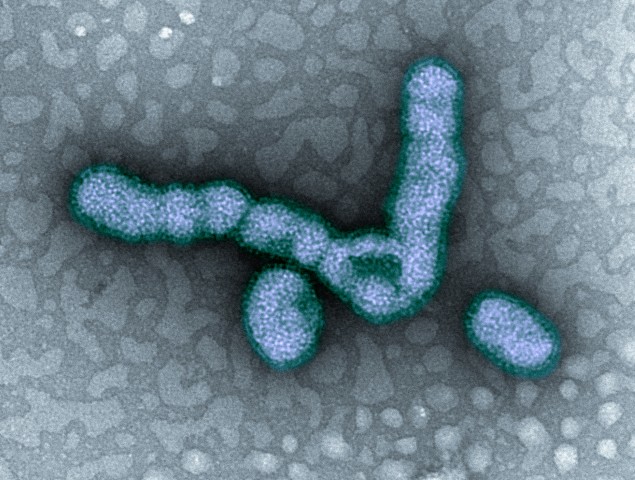
The study comes a year after reports appeared in the US Vaccine Safety Datalink showing that during the immediate period (1 to 21 days) after vaccination, older adults were suffering more strokes if they received both the Pfizer bivalent COVID vaccine and a high-dose or adjuvanted influenza vaccine on the same day.
The authors used Medicare recipient data to estimate the risk among those who received either the Pfizer or Moderna COVID-19 bivalent vaccine, concomitant (same-day) administration of either brand of COVID vaccine plus a high-dose or adjuvanted flu vaccine, and a high-dose or adjuvanted flu vaccine within the first 1 to 21-day or 22-to-42-day risk window compared with the 43-to-90-day control window. Adjuvanted vaccines include a substance that boosts immune response.
Possible stroke risk with high-dose flu vaccine
The study included 5,397,278 Medicare beneficiaries who received either brand of the COVID-19 bivalent vaccine (median age 74 years; 56% were women), 11,001 of whom had a stroke during the study period.
The authors found no significant association for stroke with either COVID vaccine, but same-day administration of either brand and a high-dose or adjuvanted influenza vaccine was associated with an elevated risk of stroke.
The observed association between vaccination and stroke in the concomitant subgroup was likely driven by a high-dose or adjuvanted influenza vaccination.
"The current study additionally found an association that was small in magnitude between stroke and administration of a high-dose or adjuvanted influenza vaccine when the vaccine was administered without concomitant administration of either brand of the COVID-19 bivalent vaccine," the authors concluded. "This finding suggests that the observed association between vaccination and stroke in the concomitant subgroup was likely driven by a high-dose or adjuvanted influenza vaccination.”