The Center for Infectious Disease Research and Policy (CIDRAP), with support from the Wellcome Trust, a London-based research nonprofit—with an eye toward improving flu vaccines, promoting truly revolutionary versions, and ensuring more equitable distribution—today released a draft of the Influenza Vaccines Research & Development Roadmap (IVR) for public review and comment.
The IVR project is being led by a steering group of scientists and policymakers and supported by a CIDRAP core team. It aims to develop a globally oriented influenza strategic planning tool to coordinate research and development (R&D), funding, and stakeholder engagement to produce more effective flu vaccines and reduce the impact of future influenza pandemics.
Begun in January 2019 and slated for full publication in summer 2021, the roadmap provides a 10-year plan with the ultimate goal of improving seasonal flu vaccines and generating new "universal" or broadly protective vaccines that are effective against a range of viral strains and provide more durable, long-lasting protection.
CIDRAP publishes CIDRAP News, but the center's news service operates independently of its research and policy efforts. See today's related commentary.
Shortcomings of current flu vaccines
Seasonal flu epidemics—caused by influenza A and B viruses—result in 3 million to 5 million annual cases of severe illness, 290,000 to 650,000 deaths, and substantial economic costs globally, according to World Health Organization (WHO) data. The burden is particularly heavy for low- and middle-income countries (LMICs) that have high rates of illness and death among the elderly and children under 5 years of age.
Flu viruses are notorious shape-shifters—mutating to produce novel strains to which people have little or no immunity—necessitating yearly reformulation of vaccines. Scientists rely on year-round surveillance to predict which strains will predominate, resulting in frequent mismatches between circulating viruses and those targeted by seasonal vaccines, and suboptimal vaccine effectiveness.
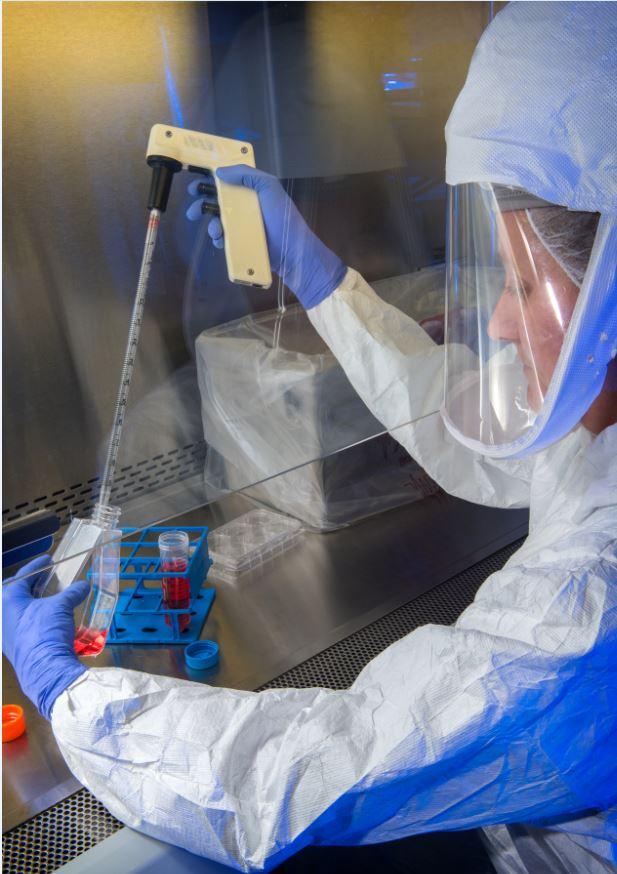
Most current seasonal flu vaccine production requires the use of fertilized chicken eggs to grow the viruses used in the vaccine. Production time constraints—a minimum of 6 months from strain selection to vaccine—limit manufacturers' ability to accurately reflect seasonal strains that circulate in a given season and also create a barrier to rapidly responding to a newly emerging pandemic strain. Viral strains used for egg-based vaccine production have also been shown to develop egg-adapted mutations that reduce vaccine effectiveness.
Even when flu vaccines are well matched to circulating strains, they do not provide lasting protection, have limited effectiveness in some populations—particularly the elderly—and do not protect against multiple or novel flu strains. Deployment of seasonal vaccines is complicated by disparities in access and inadequate national programs, particularly in LMICs.
Novel influenza viruses from animal reservoirs (mainly wild birds) can spill over to human populations, with the potential to cause severe pandemics. The 1918 flu pandemic was caused by a novel influenza A virus and is estimated to have killed 50 million people worldwide. A similar outbreak has the potential for much larger casualties today, and experts agree that future flu pandemics are certain.
The COVID-19 crisis has highlighted the severe health and economic consequences that can result from a pandemic, demonstrating the need for better flu pandemic preparedness.
Origin of the influenza roadmap concept
"Over the last 10 years, there has been an increasing awareness of the insufficiency of our current seasonal influenza vaccines," said Martin Friede, PhD, coordinator of the WHO Initiative for Vaccine Research and IVR steering group member. "This really came to a head during the 2009 H1N1 influenza pandemic," Friede added.
The H1N1 crisis, with more than 60 million cases and 12,000 deaths in the US alone, laid bare the inadequacies of the global influenza response and led to the 2017 formation of the Global Funders Consortium for Universal Influenza Vaccine Developmenta group of vaccine scientists and stakeholders. Consortium members published a list of priorities in 2019, including the need for a common landscape among funders and stakeholders to guide influenza R&D, foster open sharing of information, and to serve as a tool for advocacy and funding of vaccine development—an influenza vaccine roadmap.
"We all felt that the development of next-generation influenza vaccines was a global priority for public health and that it was going too slow—in part because the work was disjointed," said Joseph Bresee, MD, of the Centers for Disease Control and Prevention (CDC) and the Task Force for Global Health, and IVR steering group member, describing early stakeholder meetings.
"We felt that if you could take the work going on in all of the research labs, national governments, vaccine labs, and industry and align it along a single consensus roadmap, it would allow us to identify gaps that are slowing down the field in the development of life-saving vaccines and create an ecosystem in which the resources of the various stakeholders are used more efficiently over time, allowing us to get to the end result more quickly," Bresee added.
"One of the great challenges was that nobody really knew what is it that we're trying to achieve," said Friede. " Without knowing what we're trying to get to and where we are, it's pretty difficult to get there," he said.
Friede noted that one of the most important aspects of the roadmap is the coordination made possible by a shared vision. "Consensus on what it is that we're trying to achieve. Consensus on what barriers on the road are. Consensus on the steps that need to be taken to address those barriers," he said.
The Global Funders Consortium identified CIDRAP, led by epidemiologist Michael Osterholm, PhD, MPH, as the ideal organization to lead the development of the roadmap. "It didn't take more than a nanosecond of discussion," said Friede, of WHO. He pointed to CIDRAP's experience developing roadmaps for other priority pathogens including Ebola, using WHO methodology as a factor in CIDRAP's selection, as well as Osterholm's leadership in highlighting the weaknesses of the global response during the 2009 H1N1 pandemic.
Led by a steering group that includes senior leaders from the WHO, the Wellcome Trust, the Sabin Vaccine Institute, the Bill and Melinda Gates Foundation, and the Task Force for Global Health, the IVR also includes international scientific experts, subject matter experts, and other stakeholders as key members of its task force and consultation group.
IVR goals: Universal flu vaccines, durable immunity
The IVR draft released today provides a comprehensive 10-year framework for accelerating and prioritizing R&D efforts to produce universal flu vaccines that would offer robust protection against all influenza A and B viruses as well as emerging zoonotic (animal-origin) flu viruses.
 The IVR also anticipates vaccine production using "next-generation" strategies that might involve new vaccine platforms—like messenger RNA, which was used in producing the Pfizer and Moderna COVID vaccines—or that target antigens that provide longer-lasting immunity.
The IVR also anticipates vaccine production using "next-generation" strategies that might involve new vaccine platforms—like messenger RNA, which was used in producing the Pfizer and Moderna COVID vaccines—or that target antigens that provide longer-lasting immunity.
"Key components of the IVR include determining critical issues and challenges for improving influenza vaccines, prioritizing research activities, and identifying a set of realistic goals and aligned milestones in key topic areas," the roadmap authors wrote. "The IVR also offers a global perspective, taking into account the potential for different needs regarding influenza vaccine characteristics in different populations, economies, and geographic regions."
The IVR details a comprehensive list of research gaps, barriers to progress, goals, and milestones related to a broad range of topics—virology, immunology, vaccinology for seasonal and universal/broadly protective vaccines, animal and human infection models for viral research, as well as policy, financing, and regulation. The document also provides a framework for stimulating financial investment, building consensus and communication across a wide range of stakeholders, and tracking and monitoring progress over time.
"One of the goals of this roadmap effort is to lay out what R&D needs to be done," said Ed Belongia, MD, of the Marshfield Clinic in Wisconsin and roadmap subject matter expert. "We need to lay that out in as much detail as possible so that funding agencies, governments, and industries all have a coherent vision of where we need to go and what the priorities should be over the next few years to move us in the direction of more highly effective flu vaccines that are more broadly protective against different strains."
Intended as a living document, the IVR will be updated periodically as new information becomes available—some of which will certainly arise out of the COVID-19 vaccine development experience. The IVR draft will be widely disseminated to stakeholders, influencers, and experts during the public comment period, followed by further revisions, publication of the final version (May-June 2021), and IVR implementation beginning in summer 2021.
"This public comment period is the next step in our stakeholder engagement strategy," said Kris Moore, CIDRAP medical director and IVR project director. "We are now casting a wide net to those involved in influenza vaccine R&D and hope to garner important feedback that will strengthen the next iteration of the IVR."
Toward global equity
A central and intentional focus of the IVR is to improve global equity in the development and distribution of flu vaccines. Building public and government support for flu vaccination in countries with limited resources is a particularly difficult challenge.
"When countries spend very little on health, having to vaccinate the population year after year, or even subsets of the population, is a huge challenge for health budgets," said Gagandeep (Cherry) Kang, MBBS, MD, PhD, professor of gastrointestinal sciences at the Wellcome Trust Research Laboratory of the Christian Medical College in Vellore, India, and IVR task force member. "If we had better vaccines and better surveillance, it would be easier to make the case that this is important," she noted.
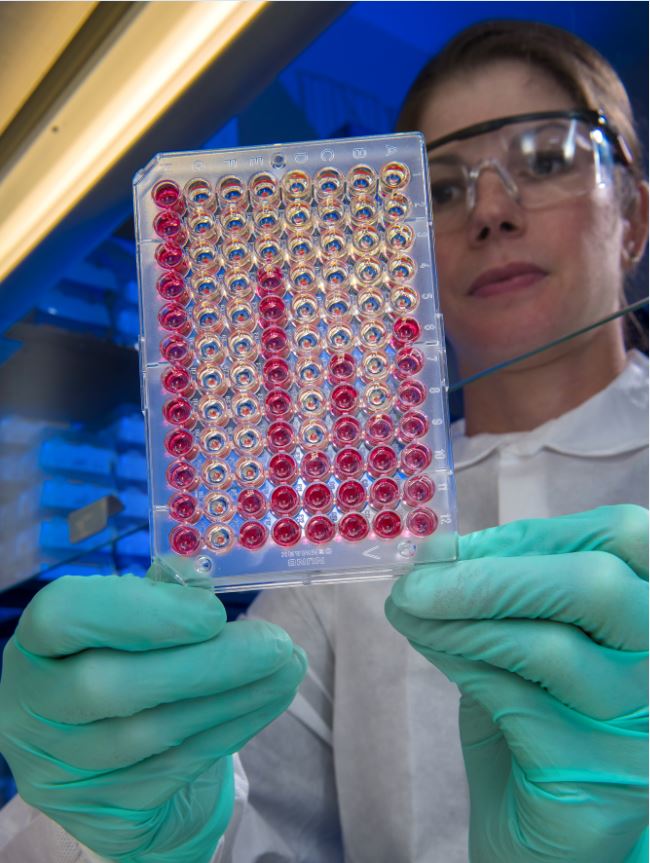
Kang highlighted the IVR's prioritization of human challenge flu studies in diverse populations around the world, noting that influenza is a disease for which prior exposure plays a role in vaccine response. She also pointed to the IVR's advocacy for the availability of standardized assays and reagents as a potentially groundbreaking development for equity in influenza research.
"Standardization is always a challenge," Kang added. "Previously, it's been dealt with by taking all the samples and moving them to a centralized lab somewhere in a developed country. And there is now a push-back—and rightly so I think—from LMICs saying that we don't want you to give us the answers or come up with the solutions. We want to build the vaccine in our own country. The IVR's aim of trying to have standardized reagents available will be very important in the future of influenza research."
The IVR also has the potential to narrow the vaccine availability gap between high-income nations and LMICs. "The roadmap is explicitly targeted to ensuring that next-generation vaccines are more quickly employed by LMICs," said Bresee, of the CDC. "We all recognize that vaccines reach people in high-income countries much more quickly than in LMICs."
"The roadmap offers a very intentional plan to ensure that the gap between availability of these new vaccines in low-income and high-income countries is diminished," Bresee added. "That increasingly is a public health goal, and we see that playing out in a very real way in the COVID-19 vaccination space. The roadmap, by acknowledging the special needs of LMICs, will do a great service to reducing the lag time between availability in high-income and low-income countries."
Streamlining funding
By identifying key R&D priorities and serving as a tool to measure progress, the IVR has the potential to increase funding efficiency, minimize redundancies, and streamline vaccine development efforts.
"It makes it easier for funding agencies to buy into this, because now we have a structure that lines up what needs to be done," said Florian Krammer, PhD, professor of vaccinology at the Mount Sinai Icahn School of Medicine and IVR task force member. "You have something you can measure. This is important for funding agencies, because they want to see what's done with their resources, and they want to see progress, and the roadmap lays out how to measure that very well."
"The roadmap will help bring together the wide variety of stakeholders involved in R&D, including national government partners like NIH [US National Institutes of Health], industry, academics, and other partners so that we can identify the key gaps or challenges that are slowing down the field of flu vaccine development, allowing public health groups, philanthropies and national governments to be able to invest more wisely," noted Bresee.
COVID-19 brings urgency to flu vaccine research
The COVID-19 pandemic has led to a paradigm shift for vaccine research, with greater public awareness of the need for vaccines bringing spillover implications for flu research. "Now everybody gets the feeling that this is something important," said Krammer. "That preparing better for a pandemic is not just something that scientists say we should do."
"What's going to be very important is that governments will have seen that a pandemic can destroy your economy within a few months," added Friede, of the WHO. "Previously when we were trying to get governments to invest even 0.01% of the [gross domestic product] on vaccine research, it was very difficult. I think that's going to change now."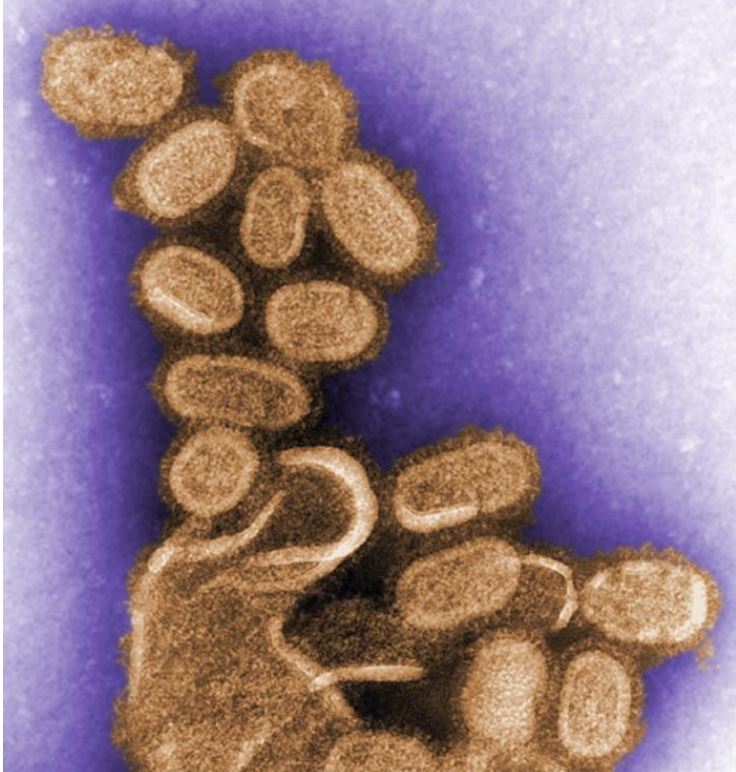
Experience gained through the COVID-19 crisis may also facilitate the execution of IVR goals. "In almost every part of the roadmap, the experience and expertise gained in COVID-19 vaccine development and implementation will make the implementation of the influenza roadmap easier," said Bresee.
"Everything will be faster," he said. "We'll have experience gained in new technologies, but we'll also have experience gained in implementing vaccinations for adult populations in many countries for the very first time. Both of these experiences will accelerate the accomplishments of the steps of the roadmap."
"I'm very hopeful that by next summer we will be at the tail end of the pandemic as we have a higher and higher proportion of the population vaccinated so that we can start to emerge from crisis mode and begin to think more proactively about where we are going to go next," said Belongia, of the Marshfield Clinic. "This certainly needs to be one of the priorities," he added, referring to the goals of the IVR project.
The lessons of COVID-19 provide a clear directive for influenza researchers, according to Kang, of Christian Medical College. "We have had a pandemic coronavirus," she noted. "We could easily have a pandemic influenza. And if we had all the tools in place for a pandemic flu—which we can relatively easily do with IVR—we can at least increase our chances of success. It will put us in a much better position for the next pandemic."
Building a broad constituency
Steering group members, task force members, and subject matter experts stressed CIDRAP's convening power as central to the IVR's success, by bringing together diverse stakeholders in a highly consultative process.
Kang noted that CIDRAP's ability to build a broad constituency, combined with the authority and expertise of the participants, gave the process a great deal of credibility. "I don't think if it had been a government-led initiative, that it could have been done in quite the same way," she noted.
"CIDRAP brings both an experience in developing these roadmaps and a passion for supporting global public health that really shows through in the dedication to this project," Bresee added. "All of us who are outside CIDRAP and have had the opportunity to support this work have been amazingly impressed by how well this project has been directed amidst all the pandemic work going on alongside it."
"Stakeholder engagement is critical to the success of the roadmap," said Moore, of CIDRAP. "By engaging a task force of experts and holding a series of consultative webinars in fall 2020 with invited experts, we have worked to ensure that the roadmap accurately reflects current R&D needs in the influenza vaccine space."
"Once the IVR is finalized and launched in June 2021, we still have a great deal of work to do toward ensuring that the priority milestones identified in the roadmap are implemented," she added. "We don’t want this document to just sit on a shelf and be forgotten."
"We hope to actively work with our IVR steering group and task force to engage the appropriate partners and help secure the necessary funding to bring the IVR to life," Moore said. "We will be monitoring progress and identifying barriers over time, along with ways to overcome them.
"We intend for the IVR to be a living document that is updated and revised as new information becomes available."