- North Carolina's health department on July 28 warned residents about the risk from exposure to saltwater or brackish water in people who have wounds or cuts, following three Vibrio vulnificus deaths in July. In a statement, the North Carolina Department of Health and Human Services said two of the people had scratches that were exposed to brackish water in North Carolina, and the third was exposed in another East Coast state. The third patient had eaten seafood that he or she had caught. No links have been found among the patients or the areas where they were likely exposed. North Carolia has reported 47 such cases since 2019, 8 of them fatal. Vibrio bacteria are normally found in warm sea water or brackish water. Aside from the risk of exposure from open skin, the bacteria can cause disease in people who eat undercooked oysters and shellfish.
- The Georgia Department of Public Health (GDPH) on July 28 reported the death of a Georgia resident from Naegleria fowleri, an amoeba that can cause rare brain infections. The patient was probably infected while swimming in a freshwater lake or pond in Georgia. The GDPH said about three such infections, typically fatal, are reported in the United States each year. Since 1962, Georgia has reported six Naegleria fowleri infections. Health officials urged people to avoid diving or jumping into bodies of warm fresh water, especially in the summer, and to avoid getting water up the nose while swimming in freshwater lakes or ponds.
- Marking its first two mosquito-borne illness detections of the year, the Michigan Department of Health and Human Services on July 28 reported two Jamestown Canyon virus (JCV) cases, one from Oakland County and one from neighboring Macomb County. Officials said mosquito pools in Bay, Saginaw, and Washtenaw counties have tested positive for JCV this summer. The Centers for Disease Control and Prevention (CDC) said about 17 neuroinvasive JCV illnesses are reported each year. It added that most infections occur between April and September. JCV is found throughout much of the country, but Minnesota and Wisconsin have reported more than half of the cases.
Quick takes: Vibrio deaths in North Carolina, Georgia reports Naegleria fowleri death, Jamestown Canyon virus cases in Michigan
NIH launches phase 2 long-COVID treatment trials
The National Institutes of Health (NIH) today announced the launch of a series of phase 2 clinical trials to assess clinical treatments for long COVID, part of a plan to test even more treatments in the months ahead.
In a statement, the NIH said the first phase 2 trials will evaluate at least four treatments, part of its ongoing RECOVER (Researching COVID to Enhance Recovery) initiative, a $1.5 billion effort that was included in the American Rescue Plan Act of 2021. One of the trials focuses on virus persistence and will evaluate longer-duration use of Paxlovid (nirmatrelvir and ritonavir) than is currently used for acute COVID infection.

Another will look at treatment of neurologic long-COVID symptoms, such as brain fog and memory problems. The interventions to be tested are a brain-training program from Posit Science Corp. called BrainHQ, a web-based goal-management program developed by the Mount Sinai Health System called PASC-Cognitive Recovery, and a home-based transcranial stimulation device developed by Soterix Medical.
A two-pronged study will evaluate treatments for sleep problems, one of them looking at two wakefulness-promoting drugs to help with excessive daytime sleepiness and the other to evaluate interventions to target problems with falling and staying asleep.
To examine treatments for autonomic system problems, the initial trial will focus on postural orthostatic tachycardia syndrome, which manifests as irregular heartbeat, dizziness, and fatigue. It will have multiple study arms, the first comparing immune system treatments with placebo and the second looking at a drug currently used to treat people with chronic heart failure.
The NIH said a fifth platform will be added and will focus on exercise intolerance and fatigue. Patients and scientists are giving the NIH input on the development of the protocol.
Rachel Levine, MD, assistant secretary for health at the Department of Health and Human Services, said in a NIH statement that the clinical trials are part of a whole-of-government response to long COVID.
"Coupled with adequate supports and services, access to clinical care and up-to-date information on what we know about long COVID, we can work toward relief for individuals and families impacted most."
Trials will launch and enroll patients on a rolling basis at clinical sites throughout the United States, the NIH said.
Rapid diagnostics, algorithm-based stewardship tied to fewer antibiotics for Staph bacteremia
Using rapid diagnostic tests (RDTs) and algorithm-based stewardship recommendations to manage coagulase-negative Staphylococcus bloodstream infection (CoNS BSI) was associated with a significant reduction in antibiotic days of therapy, researchers reported today in Open Forum Infectious Diseases.
For the study, researchers from Rutgers University and the University of Pittsburgh analyzed consecutive patients with blood cultures positive for Staphylococcus species over three independent 4-month periods. The first period was prior to implementation of RDTs, the second was a post-RDT/pre-algorithm period, and the third was a prospective post-RDT/post-algorithm period.
The aim was to see whether rapid identification of CoNS, which is a common blood contaminant but doesn't always cause BSIs, combined with an algorithm-based stewardship approach, could lower rates of antibiotic use.
A total of 182 patients with CoNS bacteremia were included in the study, with 65 in the pre-RDT period, 60 in the post-RDT/pre-algorithm period, and 57 in the post-RDT/post-algorithm period. Overall, 69%, 19%, and 12% of cases were classified as simple, uncomplicated, or complicated cases of CoNS bacteremia, respectively.
Significant reduction in antibiotic days of therapy (DOT) were observed in the post-RDT/post-algorithm period but not in the post-RDT/pre-algorithm period. While median DOT did not vary significantly for patients with simple, uncomplicated, or complicated bacteremia between the first two periods, median DOT was reduced to 0 for simple CoNS BSIs during the post-RDT/post-algorithm period.
The percentage of patients who received antibiotics for less than 24 hours rose from 33% in the first two periods to 54% in the post-RDT/post-algorithm period, and antibiotics were avoided entirely in 28% of CoNS cases in the post-RDT/post-algorithm periods, compared with 15% in the first two periods.
Pairing [rapid diagnostic tests] with early algorithm-based management can significantly reduce healthcare resource utilization.
The overall 30-day, all-cause mortality rate (14.2%) did not vary across cohorts.
"These data have major implications considering that even with robust stewardship efforts and targeted communication, nearly 87% of patients with contaminated blood cultures receive antibiotics for an average of 7 days and stay in the hospital for a median duration of 7 days," the study authors wrote. "Thus, pairing RDT with early algorithm-based management can significantly reduce healthcare resource utilization."
Study highlights threat of Staph epidermidis in ICU patients
A study of patients in two intensive care units (ICUs) suggests Staphylococcus epidermidis bacteria are an underrated cause of bloodstream infections and septic shock, French researchers reported last week in the International Journal of Infectious Diseases.
Although S epidermidis is considered a low virulence pathogen, it frequently colonizes the skin and mucous membranes and can cause infections, particularly in immunosuppressed patients with indwelling devices. To get a better sense of the clinical repercussions and prognosis of S epidermidis bloodstream infections (SE-BSIs), along with levels of antibiotic resistance, researchers conducted a retrospective study on ICU patients at two French hospitals, focusing on their epidemiologic characteristics and clinical outcomes following SE-BSIs.
A total of 59 patients with SE-BSIs were included in the study (58% men, median age of 67 years). Most patients (56%) were immunocompromised, including 44% active cancers and 17% organ transplant patients, and all but one patient had a central venous access device during their ICU stay. Of the patients, 63% required norepinephrine, a first-line agent recommended during resuscitation for septic shock, at the time of positive blood cultures, with no indications of concurrent infections.
Patients with hemodynamic consequences of SE-BSI required more mechanical ventilation at the time of bacteremia (49% vs 18%) and had a higher mortality rate (46% vs 14%). Clinical isolates were 100% susceptible to vancomycin but only 71% susceptible to linezolid.
The study authors say further research is needed to investigate host-related factors and other factors associated with S epidermidis virulence.
"Ultimately, these data should lead to clinical trials aimed at testing new anti-infectious strategies against SE-BSI," they wrote.
Study shows proctitis as predictor of mpox among symptomatic men
Proctitis was the strongest predictor of clinically confirmed mpox in thousands of patients with suspected illness who presented for testing, according to a new study in Clinical Microbiology and Infection.
The study was based on patient findings in Mexico during the global mpox outbreak, and all test results were reported to and confirmed by the Mexican Ministry of Health (MMH). Between May and November of 2022, 5,078 people were reported with mpox-like illness to MMH.
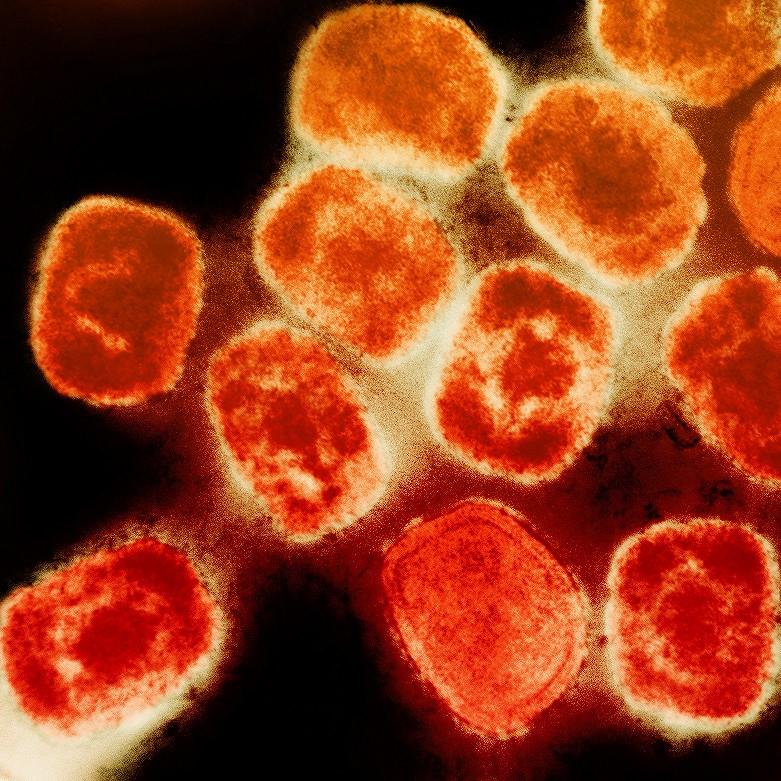
Among those, 3,291 or 64.8% were confirmed to have mpox. The strongest clinical predictor of a positive mpox test was proctitis (odds ratio [OR], 6.54; 95% confidence interval [CI], 5.93 to 7.21).
Of note, the authors said, one-third of patients who presented with pustules, genital pain, or other symptoms did not have mpox, thus suggesting that testing for other sexually transmitted infections remains important when mpox is suspected.
A second study in Emerging Infectious Diseases suggests asymptomatic mpox cases are likely underestimated. The study was based on clinical findings among men who have sex with men (MSM) in Tokyo.
By December 2022, only 8 mpox cases had been confirmed in Japan, the authors said, but since the beginning of 2023, the number of new mpox cases has steadily increased. To gauge if asymptomatic transmission was at play in the rising case counts, the study authors tested 1,346 participants for mpox, all of whom were asymptomatic.
Five of the men tested positive for the virus (0.37%; 95% CI, 0.12 to 0.86).
"Although the specific infectivity of asymptomatic cases has not yet been determined, the potential prevalence of undetected asymptomatic mpox cases could contribute to the current global pandemic," the authors concluded.










