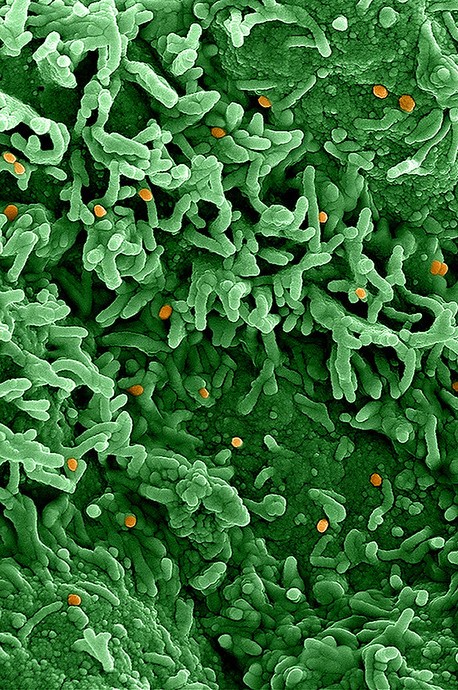
The Chicago area is experiencing a resurgence in mpox infections, which are at the highest level since November and mark the highest weekly case rate in the nation, Howard Brown Health said in a May 5 press release.
The agency, which serves the LGBTQ+ community, said it has confirmed seven cases since Apr 17, with results of other tests still pending. It added that, in the 3 previous months, the Chicago Department of Public Health had reported only one mpox case.
Patrick Gibbons, DO, Howard Brown’s chief medical director, said, "We urge sexually active members of our community to receive the mpox vaccine. For example, unvaccinated people planning to attend International Mr. Leather at the end of May should receive their first dose of the mpox vaccination as soon as possible." He added that increased vaccination rates will better protect the community from another outbreak.
Concerns over global resurgence
Following last year's international outbreak, cases dropped sharply over the winter months. In February, the World Health Organization kept the public health emergency of international concern (PHEIC) in place for mpox, citing sustained transmission in some countries, undetected transmission and under-reporting in others, and concerns about a possible resurgence when social events and other mass gatherings resume.
Other countries have reported upticks in mpox activity, such as a cluster in France and South Korea, where officials last month raised the alert level from 1 to 2.
 The rare cases of myocarditis among recipients of mRNA COVID-19 vaccine—mostly in young men—are caused by a generalized immune-cell and inflammatory response rather than vaccine-triggered antibodies, suggests a small
The rare cases of myocarditis among recipients of mRNA COVID-19 vaccine—mostly in young men—are caused by a generalized immune-cell and inflammatory response rather than vaccine-triggered antibodies, suggests a small  An Australian postmarketing study of
An Australian postmarketing study of  A study presented late last week at the Digestive Disease Week 2023 conference suggests that exposure to antibiotics at an early age is among the factors that can increase the risk of pediatric inflammatory bowel disease (IBD).
A study presented late last week at the Digestive Disease Week 2023 conference suggests that exposure to antibiotics at an early age is among the factors that can increase the risk of pediatric inflammatory bowel disease (IBD).











