Nov 11, 2008 (CIDRAP News) Clostridium difficile, rapidly gaining as a source of hospital-acquired infections, is sickening from 6 to 20 times more patients than previously thought, according to a survey released today by the Association for Professionals in Infection Control and Epidemiology (APIC).
Kathy Warye, APIC's chief executive officer, told reporters at a press conference today that the study is the first to reveal the true magnitude of C difficile infections in hospitals. The survey represents a 1-day snapshot of all patients with C difficile infections in 648 participating hospitals. The pathogen causes diarrhea and other, more serious intestinal problems.
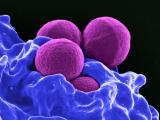
C difficile is the second most common and troublesome nosocomial infection, raking right behind methicillin-resistant Staphylococcus aureus (MRSA), she said. In 2007, APIC commissioned a similar hospital snapshot study of MRSA, which she said was a wake-up call for health officials that triggered increased attention and resources needed to slow rising illness rates.
Based on extrapolation of the results to the entire US inpatient population, the APIC authors estimated that on any given day, 7,178 patients have C difficile and an average of 301 die of it. They project that these cases lead to an average of 40,197 extra hospital days and about $32.1 million in healthcare costs.
"Studies like this can be very powerful. The time for action in now," Warye said, speaking from an APIC conference on C difficile in Orlando, Fla. The organization also released a guide for eliminating the organism, which will be published tomorrow on APIC's Web site.
Infections can be fatal
C difficile is a gram-positive bacteriumtransmitted by hand contact with objects contaminated with fecesthat causes diarrhea and potentially fatal conditions such as colitis, toxic megacolon, and sepsis, according to APIC. Infections are associated with previous antibiotic use and are most common in older patients and others who have been in hospital, nursing home, or other healthcare settings. Over the past 30 years the pathogen has emerged as one of the leading causes of infections acquired in healthcare settings.
In the past 5 years, a more virulent, antibiotic-resistant strain of C difficile has evolved, known as the North American pulse-field type 1 (NAP1).
William Jarvis, MD, principal investigator for the study and president and cofounder of Jason and Jarvis Associates, a healthcare epidemiology firm, told reporters previous studies on C difficile rates were incidence studies based primarily on patient discharge data. For example, he said two earlier studies revealed 60 and 76 ill patients, respectively, per 10,000 discharges.
The previous studies are limited because they captured only a small amount of data over a long period of time, he said.
Jarvis said the current survey gauges prevalence and was able to capture detailed clinical information that helped reveal patterns about the patients' illness. APIC members were asked to collect data on all of their patients with C difficile patients on one day between May and August 2008. The survey covered 12.5% of all medical facilities in the United States and reflected broad patient populations.
Jarvis and his colleagues found that 13 of every 1,000 patients covered in the survey were either infected or colonized with C difficile, for a total of 1,443 patients. Most (94.4%) were infected.
Illness patterns emerge
Detailed data were provided for 1,062 patients, which Jarvis said revealed some notable patterns. For example, 54% were diagnosed with C difficile infection within 48 hours after hospital admission, which initially suggested some had acquired the infection during a previous hospital stay or in the community.
Of the group, about 85% were hospitalized for other conditions, and about 68% had comorbid conditions such as renal failure or diabetes. "C difficile isn't just a surgical disease," Jarvis told reporters. Nearly 80% of the patients had been on antibiotics before they got sick with C difficile; in 17% of the cases, the antibiotics were for preventing surgical infections.
Nearly 90% of the patients were diagnosed by enzyme-linked immunoassay for A and B toxins rather than by culture, which Jarvis said points to a lack of capacity to isolate the organism and determine how many cases are caused by the drug-resistant NAP1 strain.
A hard-to-kill bug
Jarvis said study has several practical implications for infection control specialists. The spore-forming form of C difficile is one of the more difficult organisms to kill, as bleach is the only cleaner that can kill it, he said. However, only 65% of the survey participants said they used bleach to combat C difficile outbreaks.
Also, more "antibiotic stewardship" programs are needed to reduce antibiotic use in hospitals, he said. The survey showed only 50% of facilities have such programs. "We're hoping that this will be a call for action, not just for infection control experts but also hospital administrators who are in position to provide the resources," Jarvis said. "We need a bundle of practices, not just one."
For hand hygiene, he said alcohol gels won't kill C difficile spores, and vigorous hand washing with soap and water is needed to remove them.
APIC published an executive summary of the survey on its Web site, and Warye said the complete report will appear in an early spring issue of the organization's journal, the American Journal of Infection Control.
See also:
Nov 11 APIC press release
Executive summary of APIC's C difficile survey