Vaccine advisors for the Food and Drug Administration (FDA) today recommended emergency use authorization [EUA] for Pfizer-BioNTech's COVID-19 vaccine, clearing one of the last hurdles before immunization is set to begin within days for the first groups to receive it—healthcare workers and nursing home residents.
The FDA typically follows the recommendations of its independent Vaccines and Related Biological Products Advisory Committee (VRBPAC), and FDA Commissioner Stephen Hahn, MD, has said this week that the FDA will make its approval decision shortly after the meeting.
As FDA advisors took up the issue today, researchers published the peer-reviewed phase 2/3 findings in the New England Journal of Medicine, fleshing out more details about safety and efficacy. Earlier this week, the VRBPAC signaled its support for the vaccine in extensive background materials released ahead of the meeting.
The main question before the group today was whether, based on the data so far, the benefits of the vaccine outweigh the risks in people ages 16 and older. The measure passed with 17 yes votes, 4 no votes, and 1 abstention. Some who voted no weren't certain about teens ages 16 and 17 being in the initial EUA.
The experts also examined how the companies would continue their ongoing trials after the EUA, which raises issues about the loss of blinded, placebo-controlled follow-up ahead of full licensure.
The panel also addressed other issues related to the rollout of the vaccine, such as post-approval safety testing, distribution, and use in pregnant and breastfeeding women. And they pressed for more information on anaphylactic reactions that were reported in two healthcare workers on Dec 8, the first day of vaccination in the United Kingdom.
Worries about anaphylaxis, vaccine uptake
Paul Offit, MD, a VRBPAC member who is professor of pediatrics at the Children's Hospital of Philadelphia, said he worried that reports of allergic reaction in the UK health workers could influence vaccine uptake, given there are millions of people with known severe allergies carry EpiPens, and he asked the company for more information from the clinical trials.
A Pfizer official said the trial excluded people who had a history of severe reactions to a vaccine and those who had allergic reactions after the first vaccine dose. No participants had reactions after the first dose, so none were excluded from getting a second dose. He said there were no serious allergic reactions in study participants.
Another Pfizer official said the first UK patient had a history of severe food allergies and the second had a history of an allergy to a drug, but was not under the care of an immunologist.
Offit urged Pfizer to do a careful observational study in people with, for example, egg and peanut allergies, to prove there's not a problem. "This issue is not going to die until we have better data."
Marion Gruber, PhD, who directs the FDA's office of vaccines research and review, said the FDA had already added a warning to the vaccine fact sheet for people who have a history of allergy to any component of the vaccine.
Safety for pregnancy, breastfeeding
Panel members today raised concerns about the lack of data on pregnant and lactating women, who weren't studied in the vaccine trials. They urged vaccine makers to do developmental and toxicity studies in animals before launching trials in pregnant and breastfeeding women. A representative from Pfizer said the company expects data from experiments in rats by the middle of December.
Doran Fink, MD, PhD, deputy director of the FDA's vaccines and related projects division, acknowledged that many healthcare workers in the priority group are women of childbearing age who are pregnant and that the EUA wouldn't preclude them from making their own decision to be vaccinated under the guidance of their health provider.
Clarifying trial participant issues
During today's deliberations, the experts also worked through several issues that would arise, once the vaccine is approved, such as what happens next with safety monitoring. Nancy Messonnier, MD, who directs the Centers for Disease Control and Prevention's (CDC's) National Center for Immunization and Respiratory Diseases, said systems will be in place on the first day of vaccination to monitor vaccine safety.
She said the safety monitoring plan is extensive, with a whole-of-government approach that will initially focus on the first priority groups, including active surveillance of healthcare worker recipients, with rapid follow-up of serious adverse event reports.
The group also grappled with whether study volunteers who received a placebo can now receive the approved vaccine. Researchers hope that many members of the placebo group remain, so that the studies can continue.
Steven Goodman, MD, MHS, PhD, with Stanford University School of Medicine, said volunteers are free to withdraw, once the vaccine is approved and it is their turn to be immunized. For example, in the short-term, a healthcare worker trial participant—being part of the first priority group—may want to withdraw from the trial to be vaccinated.
The group also covered how the vaccines will be ordered and distributed, once approved. Anita Patel, PharmD, with the CDC's Vaccine Task Force, said all vaccines will be ordered through the CDC, which will route them to the vaccine maker for distribution to administration sites. She added that the distribution system also enables key supplies such as diluent and dry ice replacement to arrive at vaccination sites at about the same time as the vaccine.
Next steps
The EUA paves the way Operation Warp Speed to begin shipping vaccine to states, but the vaccine can't be given until the CDC vaccine advisory group recommends it. The Advisory 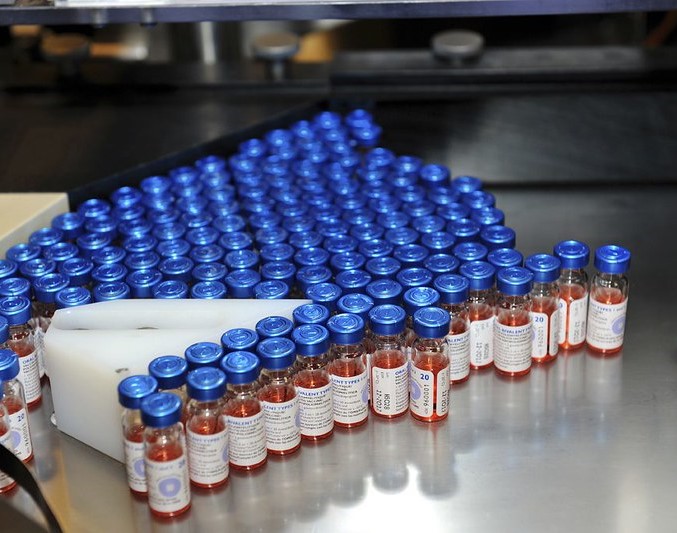 Committee on Immunization Practices (ACIP) will meet in emergency sessions tomorrow and on Dec 13 to take up the issue. The meeting agenda says the group will vote on Dec 13.
Committee on Immunization Practices (ACIP) will meet in emergency sessions tomorrow and on Dec 13 to take up the issue. The meeting agenda says the group will vote on Dec 13.
On Dec 17 VRBPAC will meet to consider an EUA application for the second COVID-19 vaccine, the one from Moderna.
A triumph with lingering questions
Commenting in NEJM on today's study, Eric Rubin, MD, PhD, an infectious disease expert, a temporary voting member of VRBPAC, and the journal's editor-in-chief, and Dan Longo, MD, deputy editor, wrote that the trial results are impressive enough to hold up to any conceivable analysis. "This is a triumph," they said, noting that the vaccine moved from conception to large-scale implementation within a year, compared to decades for most vaccines.
Rubin and Longo emphasized, however, that important questions remain, such as long-term safety, ensuring that people receive their second dose, how long protection lasts, and whether the vaccine prevents asymptomatic transmission.






















