Regeneron's combination of two monoclonal antibodies lowered the risk of COVID-19–associated hospitalization and death from any cause by 71% and resolved symptoms and reduced SARS-CoV-2 viral load faster than a placebo, a phase 3 clinical trial finds.
In the study, published yesterday in the New England Journal of Medicine, a team led by Regeneron researchers randomly assigned 2,696 adult COVID-19 outpatients at high risk for severe illness to receive either intravenous REGEN-COV or a placebo from Sep 24, 2020, to Jan 17, 2021.
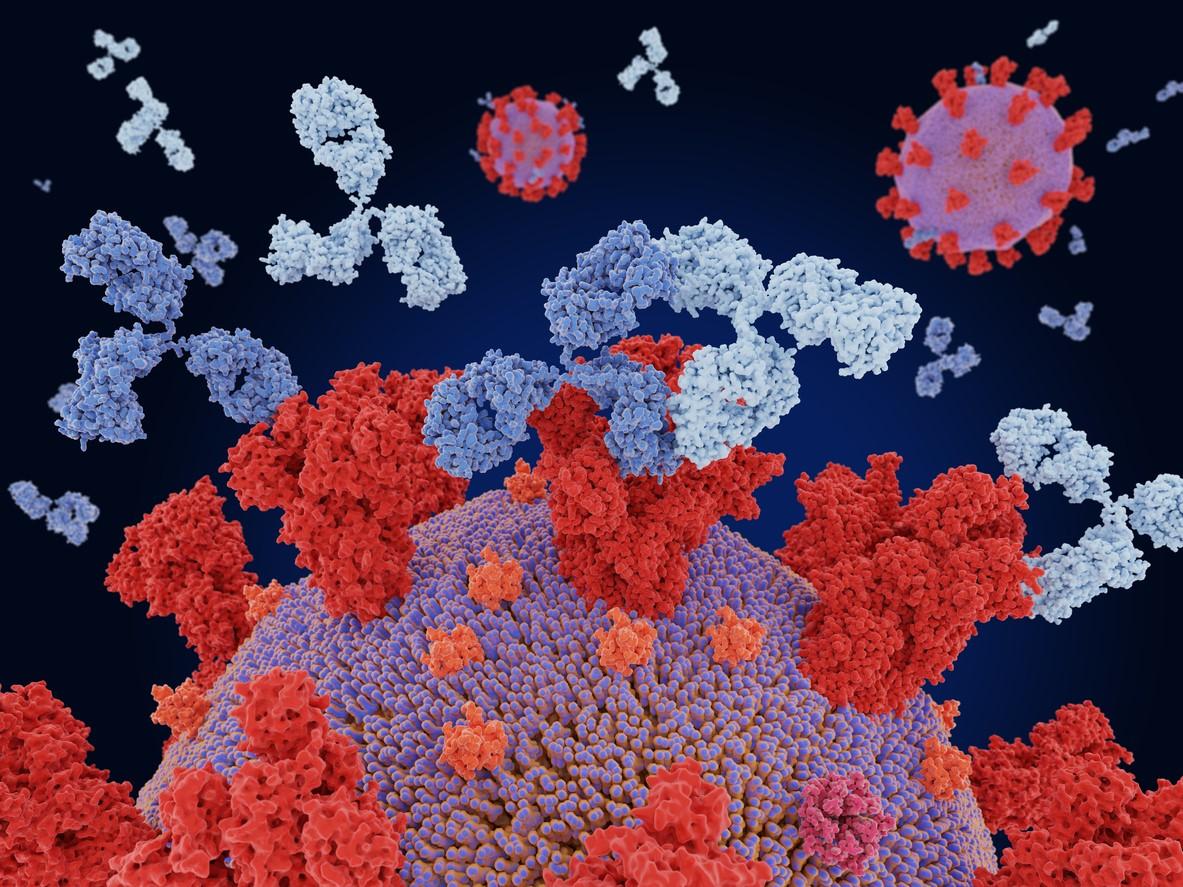
REGEN-COV is a 1:1 combination of the monoclonal antibodies casirivimab and imdevimab.
Effective regardless of baseline antibody status
Of 1,355 patients given 2,400 milligrams (mg) of REGEN-COV, 18 (1.3%) were hospitalized or died from any cause within 28 days, compared with 62 of 1,341 patients (4.6%) given placebo (relative risk reduction [RRR], 71.3%).
Seven of 736 patients (1.0%) who received 1,200 mg of REGEN-COV were hospitalized or died, versus 24 of 748 (3.2%) of the placebo group (RRR, 70.4%). The REGEN-COV group was also less likely to require intensive care unit admission.
The researchers noted that previous research has shown that REGEN-COV is effective in vitro against variants of concern, including Delta (B1617.2).
Patients given placebo who had SARS-CoV-2 antibodies at the start of the trial had a comparable incidence of hospitalization and death as those who had no antibodies, suggesting that some patients with antibodies mounted an ineffective immune response.
"Moreover, this trial showed that REGEN-COV is associated with clinical benefit, regardless of baseline serum antibody status, so that serologic testing at the time of the COVID-19 diagnosis is less critical for making clinical treatment decisions," the study authors wrote.
Faster symptom resolution, lower viral load
Symptoms in the REGEN-COV group resolved a median of 4 days faster than in the placebo group, regardless of dose (10 vs 14 days). Both doses of REGEN-COV also lowered viral load faster than placebo.
The placebo group experienced more serious adverse events (4.0%) than the 1,200-mg REGEN-COV group (1.1%) and the 2,400-mg group (1.3%). Less than 0.3% of patients in all groups had a moderate or severe infusion-related adverse reaction.
Median patient age was 50 years, 14% were 65 and older, 49% were men, 35% were Hispanic, and most had experienced symptoms for 3 days before study enrollment. The most common risk factors included obesity (58%), age 50 and older (52%), and cardiovascular disease (36%), and 3% were immunocompromised. Most (69%) had no SARS-CoV-2 antibodies at baseline, and the median viral load was high, suggesting the early phase of infection.
The phase 1/2 trial showed that the drug reduced both SARS-CoV-2 viral load and the number of medical visits and that 2,400-milligram (mg) and 8,000-mg doses had comparable antiviral and clinical efficacy.
In November 2020 the US Food and Drug Administration granted emergency use authorization to REGEN-COV for treating high-risk patients 12 and older who have moderate to severe COVID-19. The authorization was expanded for post-exposure prophylaxis in July 2021. The drug is free for eligible patients.