A media outlet in Bangladesh has reported that two men have died from Nipah virus infections, and local officials said both had consumed raw date juice—a known risk factor for contracting the disease—before they became ill. The cases are the country's first of the year.
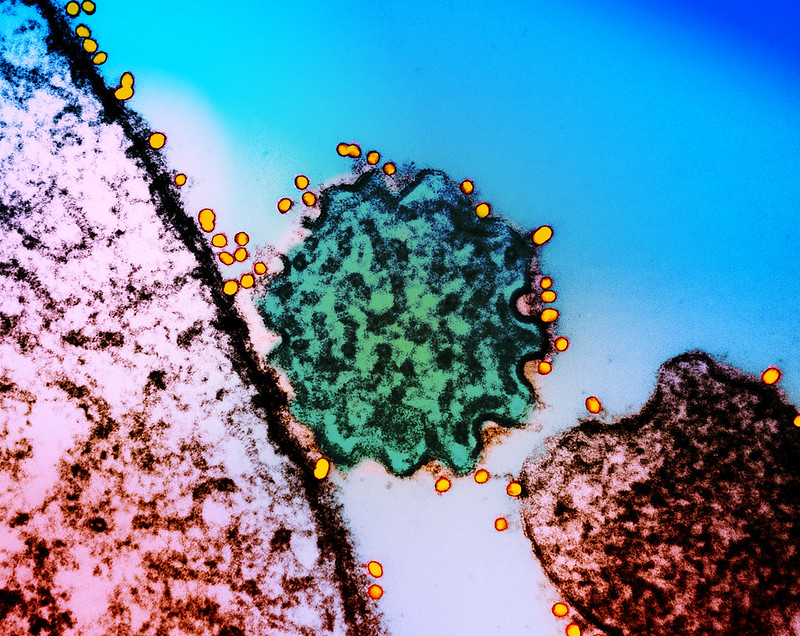
Nipah virus cases in Bangladesh follow a seasonal pattern, from December through May. The period coincides with the harvesting of palm sap and festivities related to the process. The sap can be contaminated by the saliva, urine, or droppings from fruit bats, which are thought to harbor the virus. The virus can then spread from person to person.
According to the Dhaka-based Business Post, one of the patients is a 38-year-old man who was admitted to a hospital in Manikganj district on January 16. Two days later, when his condition worsened, he was transferred to a hospital in Dhaka, where his Nipah virus infection was confirmed. The other patient is a 27-year-old man from the same district who was initially treated with products from a local pharmacy after his symptoms began and was hospitalized in Dhaka after his condition deteriorated.
Bangladesh reported 14 cases in 2023, 10 of them fatal, putting the country's deaths from the virus at their highest level in 5 years. Nipah virus infections have a high case-fatality rate, between 45% and 75%. There are no approved treatments or vaccines, and the World Health Organization has designated it a priority disease for research and development. The Coalition for Epidemic Preparedness Innovations has also prioritized Nipah virus for countermeasure development.

 In an attempt to establish a definitive objective cognitive marker for PCC, or post-COVID-19 condition, researchers tested long COVID patients in Germany and the United Kingdom with cognitive speed tests, and found long COVID patients
In an attempt to establish a definitive objective cognitive marker for PCC, or post-COVID-19 condition, researchers tested long COVID patients in Germany and the United Kingdom with cognitive speed tests, and found long COVID patients 









