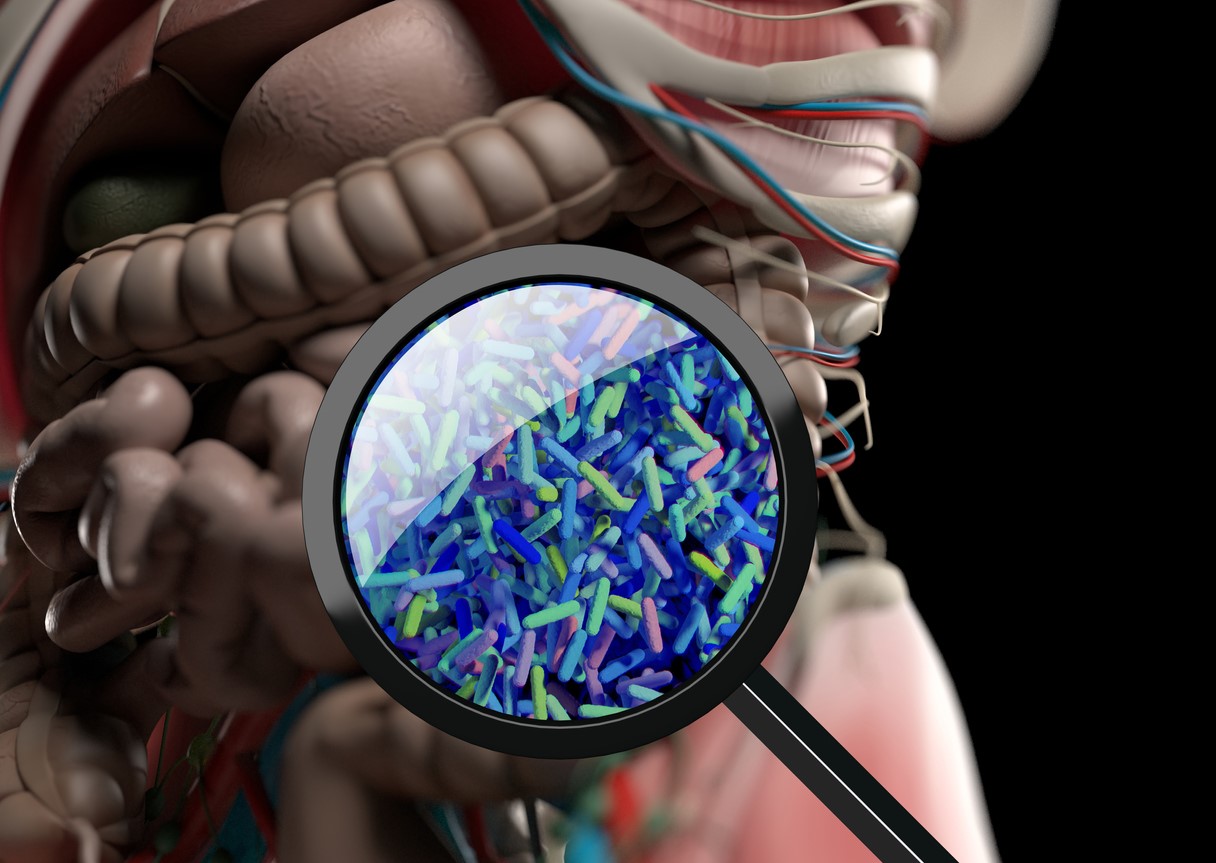
 A systematic review yesterday in PLOS Medicine found that antibiotics significantly reduced bacterial diversity and altered the gut microbiome of infants in low- and middle-income countries (LMICs).
A systematic review yesterday in PLOS Medicine found that antibiotics significantly reduced bacterial diversity and altered the gut microbiome of infants in low- and middle-income countries (LMICs).
Conducted by researchers from the University of Amsterdam and the Centre for Infectious Disease Research in Zambia, the systematic review examined studies that reported on the effects of antibiotics on the gut microbiota of children under age 2 in LMICs and profiled resistance genes. Of 92 studies assessed, 10 met the eligibility criteria, all of which were randomized controlled trials comparing children who received antibiotics with those who received placebo.
The studies were conducted in South Africa (1), Niger (4), Burkina Faso (3), India (1), and Malawi (1) and assessed a limited number of antibiotics, including cotrimoxazole (3 studies), azithromycin (9 studies), and amoxicillin (2 studies).
Overall, the studies showed that the children who received antibiotics had reduced gut microbiome diversity and increased antibiotic-specific resistance gene abundance, particularly the children who received azithromycin, in whom macrolide resistance was seen as early as 5 days post-treatment and persisted for up to 6 months. Studies on children who participated in biannual mass azithromycin distribution, a strategy that has been used in several African countries, also had a greater abundance of non-macrolide resistance determinants.
Research initiatives are urgently needed to understand how antibiotic perturbations on the microbiome translate into health benefits or risk of disease.
The authors say the findings are limited by the paucity of studies, and that several questions remain. Among them are whether depletion of commensal microbiota renders children more susceptible to infections, whether antibiotic use puts children at risk for infection with antimicrobial-resistant (AMR) pathogens, and whether disruption of the infant microbiome translates into short- and long-term health issues.
"Given the vulnerability of children in LMIC to infections, the frequency of antibiotic consumption in their early lives, and the growing global threat of infections with AMR, harmonized research initiatives are urgently needed to understand how antibiotic perturbations on the microbiome translate into health benefits or risk of disease," they wrote.