A new study based on 14 years of Nipah virus infections in Bangladesh—the country hit hardest by the disease—revealed an elevated risk to caregivers, the role of respiratory secretions, and other new clues about what fuels transmission among humans, findings that could help control future outbreaks.
An international group of researchers published its findings today in the New England Journal of Medicine.
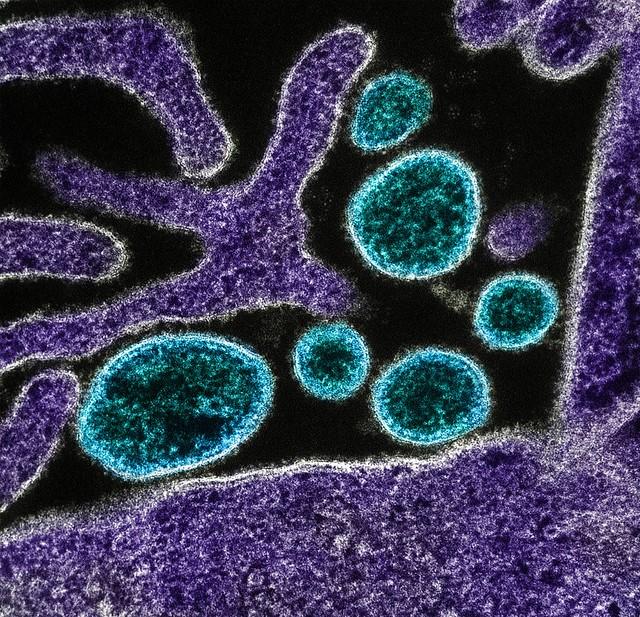
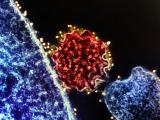
Nipah virus, a paramyxovirus spread by bats found throughout South and Southeast Asia, is one of nine World Health Organization (WHO) priority diseases for research and development.
Given its severe respiratory and neurologic symptoms, Nipah virus infections have a high case fatality. There are no treatments or vaccines for the disease, however, which in 2017 landed Nipah on a list of three diseases targeted by the Coalition for Epidemic Preparedness Innovations, a new vaccine partnership that came together in the wake of West Africa's massive Ebola outbreak.
Transmission risks, who gets sick
In their search for transmission patterns, the group studied the characteristics of all of Bangladesh's Nipah virus cases over the last 14 years and examined data for 2,000 of the patients' contacts. They used information from detailed outbreak investigations that were conducted by Bangladesh's International Centre for Diarrheal Disease Research and the country's Institute of Epidemiology Disease Control and Research. Of 248 cases, 82 involved human-to-human transmission.
The investigators found that adult patients who had respiratory symptoms transmitted the virus to more people than other case-patients. Also, contacts who were exposed to body fluids—including respiratory secretions—of sick people were more likely to become ill.
When the researchers looked at other connections among patients and their contacts, they found that spouses and contacts with long exposure duration, such as caregivers, were more likely to become infected.
Birgit Nikolay, PhD, who is at the Pasteur Institute in Paris and is the study's first author, said in a Pasteur press release, "The results of this study help identify patients that should be targeted for interventions such as isolation measures if resources are insufficient to cover all suspected Nipah cases. This may help better control the spread of the virus during large outbreaks."
The authors note that several research gaps remain, and studies are needed to clarify how the virus propagates in the human body and what criteria define Nipah virus spreaders. Also, research studies are planned to better understand when and where transmission is occurring in bats, which may help predict Nipah virus spillovers to humans.
New approaches needed
In an accompanying commentary in the same journal, Jeremy Farrar, MD, PhD, director of the Wellcome Trust, said Bangladesh has experienced a Nipah virus outbreak every year since 2001, but large gaps remain in understanding the virus, including how it crossed to India in 2018 to trigger an outbreak in Kerala.
Alluding to the WHO research priority list, which includes a yet-unknown "disease X," he said Nipah virus was disease X until 20 years ago, and to better prepare for future epidemics, the world needs to expect them.
"There is no justification for closing our eyes to such threats, hoping we'll be safe, and then panicking when we realize we're not. Nor can we treat each episode as a discrete one-off event," Farrar wrote.
Epidemic preparedness must keep pace with a host of changes, including climate, vector species migration to new areas, evolving interactions between people and animals, increasing interconnectivity and speed of travel, and political instability and conflict, he said.
Also, Farrar said preparedness and response to epidemics could be improved by clearer definitions of the relationships between countries, the WHO, and other global health groups, as well as more innovative approaches to funding essential work on fighting viruses.
See also:
May 9 N Engl J Med study
May 8 Pasteur Institute press release
May 9 N Engl J Med commentary