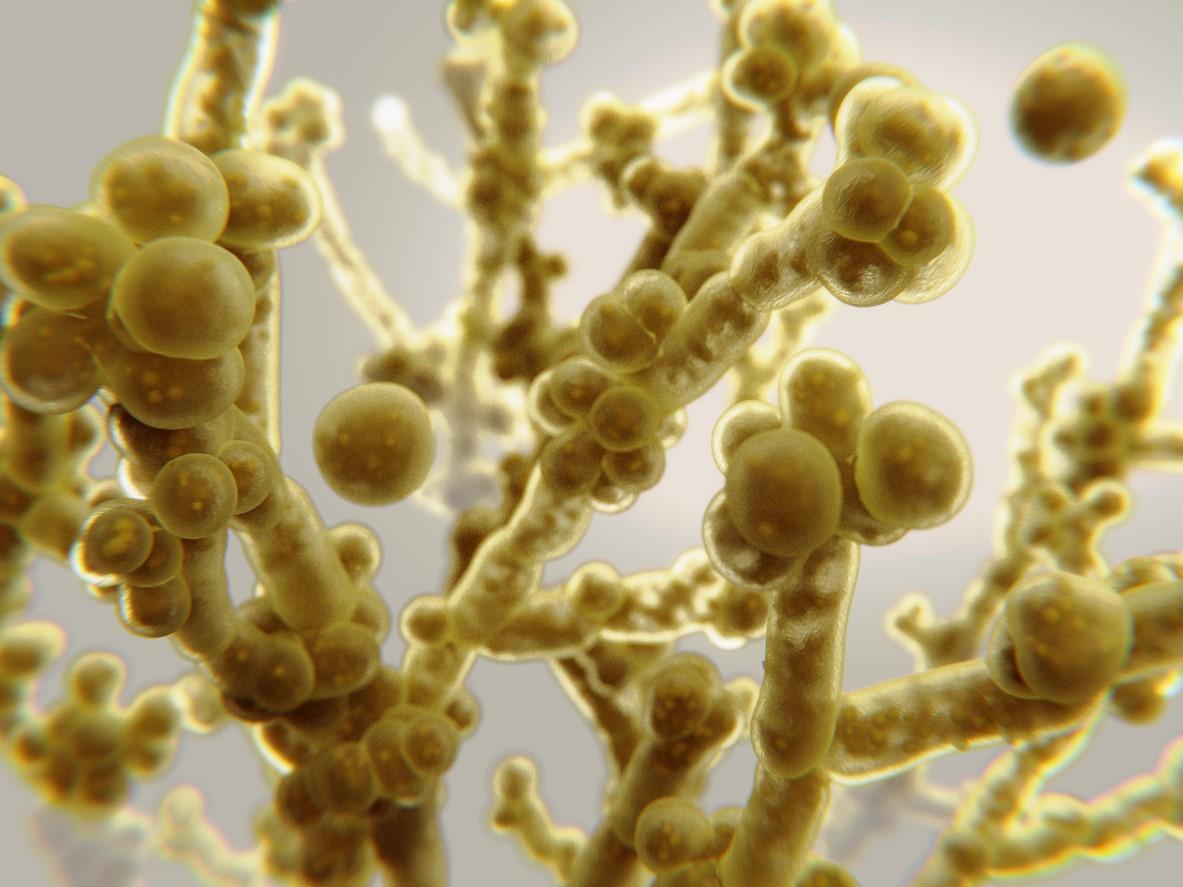
The World Health Organization (WHO) said today in an outbreak notice that 13 countries in Africa have reported confirmed or probable yellow fever cases since the start of 2023. It urged countries to increase surveillance because of the potential for onward transmission through travel and the presence of mosquitoes in neighboring countries that are capable of spreading the disease.

The countries are Burkina Faso, Cameroon, the Central African Republic, Chad, Republic of the Congo, Ivory Coast, the Democratic Republic of the Congo (DRC), Guinea, Niger, Nigeria, South Sudan, Togo, and Uganda. During the last quarter of 2023 through February 25, eight of the countries have reported active yellow fever transmission and have started response planning: Cameroon, Chad, Congo, DRC, Guinea, Niger, Nigeria, and South Sudan.
Niger and Nigeria reported cases in January, and investigations are still under way. An outbreak in South Sudan, first reported in December 2023 and centered in West Equatoria state, has grown to 64 cases that fit the case definition, of which 6 were fatal.
Urban spread in Cameroon's biggest city
The WHO also warned that Aedes mosquitoes in urban areas can amplify outbreaks. It said that, of Cameroon's nine lab-confirmed cases, six were from a densely populated area of Douala, the country's largest city.
Preliminary information for 2023 shows a case-fatality rate of 11%.
Though progress has been made with vaccination, suboptimal vaccine coverage in some areas and persistent population immunity gaps pose a high risk and threaten progress toward elimination. The WHO put the regional risk at moderate and kept the global risk low.