When it comes to antibiotic resistance, history matters.
That's the message of a new study in PLoS Biology by two scientists from the University of Virginia (UVA) that investigated how the history of resistance to one antibiotic can influence resistance profiles when bacteria subsequently adapt to another antibiotic. The results demonstrate that the way bacteria have adapted to antibiotics in the past can change their evolutionary path moving forward, influence how resistant they become to new antibiotics, and affect overall resistance profiles.
While the experiments were done in a controlled laboratory setting, the hope is that understanding the history of bacterial adaptation could one day help clinicians design treatments for bacterial infections that limit the development of antibiotic resistance, especially multidrug resistance.
"These history-specific effects have direct clinical implications on optimizing antibiotic treatment strategies to slow and prevent the emergence of dangerous multidrug-resistant bacterial pathogens," the authors write.
Adaptive laboratory evolution
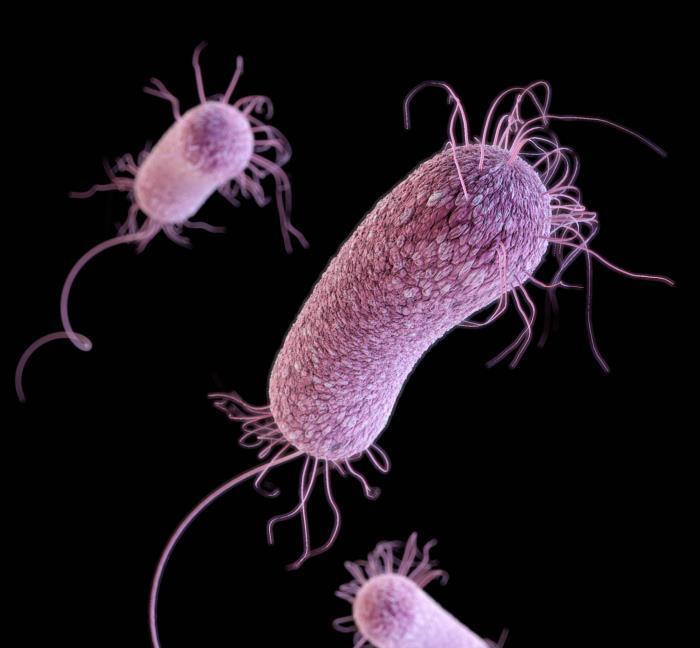
In the study, Jason Papin, PhD, a professor of biomedical engineering at UVA, and his colleague, Phillip Yen, PhD, took laboratory samples of the bacterial pathogen Pseudonomas aeruginosa and observed its adaptation to different two-drug sequences of the three antibiotics commonly used to treat P aeruginosa infections—piperacillin, tobramycin, and ciprofloxacin. In each sequence, the bacterium was subjected to 20 days of adaptation to increasing concentrations of an initial drug, then subjected over the next 20 days to one of the other three drugs.
The aim of the approach they were using, known as adaptive laboratory evolution, is to study the evolutionary path of bacteria as they adapts to antibiotic pressure over time. "The primary objective is to evolve the bacteria in a highly controlled way…so that you can try to understand the mechanisms associated with that evolutionary process, and the resulting phenotypes [levels of resistance] that emerge" Papin said in an interview.
In this series of experiments, what Papin and Yen wanted to observe was whether resistance to each of the three drugs changed depending on the different drug sequences, and how it changed—what they call the drug-order-specific effects. What they found, Papin explained, is that resistance isn't just a response to a current drug regimen but also depends on past regimens. "The high-level message is that order matters, and history matters," he said.
For example, when P aeruginosa lineages that had initially become resistant to tobramycin over 20 days were subsequently adapted to ciprofloxacin over the following 20 days, they became less resistant to tobramycin. The same thing happened, to a lesser extent, when the tobramycin-adapted lineages were exposed to piperacillin. And when ciprofloxacin-resistant lineages were adapted to both piperacillin and tobramycin, they became less resistant to ciprofloxacin.
These examples demonstrate that resistance to a drug might be reversed by treatment with a second drug. But whether this happens depends on the sequence of the drugs. When piperacillin-resistant P aeruginosa was evolved to tobramycin, for example, piperacillin resistance remained high. Translated into a clinical setting, that could mean that a P aeruginosa infection that was treated first with piperacillin and then with tobramycin could become multidrug-resistant.
In addition, Papin and Yen found that a history of adaptation to one drug can affect the rate at which resistance can arise when a bacterium is adapted to a second drug. This was observed when initial adaptation to piperacillin was found to slow down the subsequent evolution of resistance to tobramycin. The researchers also found that a two-drug sequence could result in a different overall resistance profile, depending on which drug was used first.
Clinical impact
The study acknowledges that many clinically important factors involved in the emergence of antibiotic resistance, such as pathogen-host interactions and the role of horizontal gene transfer, were not considered in the study, and that actual clinical studies need to be performed to test the true clinical applicability of the results. And Papin is careful to note that the clinical applicability of adaptive evolution, at this point, is theoretical. But he does think the concept could have clinical relevance.
"When we understand what those history-dependent effects are, we could build an awareness of which sequences of antibiotics are going to either be advantageous or be detrimental for a particular bacterium a clinician might be dealing with," he said. "That's kind of a pie-in-the-sky idea of where this could go."
See also:
Aug 8 PLoS Biol study