A new report from the Canadian Antimicrobial Resistance Surveillance System (CARSS) shows rising antibiotic resistance in two major healthcare-associated pathogens, along with noteworthy decreases in antibiotic use in humans and animals.
The CARRS-2017 Report is the third published by the Public Health Agency of Canada (PHAC) and includes surveillance data on antimicrobial resistance and use, both in humans and animals, through 2016. The report is based on available surveillance data from the PHAC's nine surveillance systems and laboratory reference services. This year's report includes new data on antibiotic-resistant infections and antibiotic use in community settings.
Worrisome trends
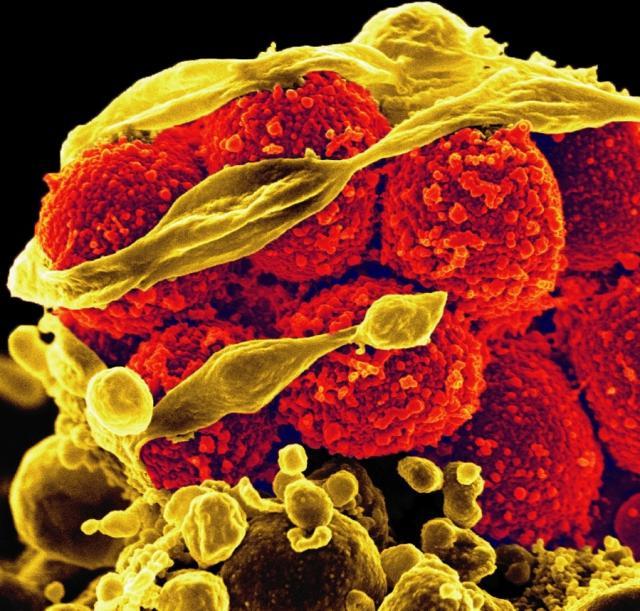
The two pathogens of concern are methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE). The CARRS report shows that the overall rate of MRSA infection in sentinel hospitals in Canada increased from 2.84 cases to 3.13 cases per 10,000 patient-days from 2011 through 2016, with a decrease in healthcare-associated MRSA (HA-MRSA) cases (from 1.93 cases in 2011 to 1.69 in 2016) and an increase in community-associated cases (from 0.56 cases to 0.96 cases per 1,000 admissions).
Most concerning was a fivefold increase in HA-MRSA bloodstream infections (BSIs) in the country's pediatric hospitals—from 0.08 to 0.43 cases per 10,000 patient-days between 2011 and 2016.
The rate of VRE infections in Canada, meanwhile, rose from 0.41 cases per 10,000 patient-days in 2015 to 0.44 cases in 2016. While that's a reduction from a high of 0.61 cases in 2012, it still represents a significant rise since 2007, when the rate was 0.10 cases per 10,000 patient-days. In addition, the report shows that the rate of VRE BSI in sentinel adult hospitals more than doubled from 2011 to 2016, climbing from 0.12 cases per 10,000 patient-days to 0.26 cases. "This finding points to the need for ongoing monitoring of this microorganism in Canada," the authors of the report write.
The report also found that drug-resistant gonorrhea is becoming an increasing problem in Canada, matching a trend that has been observed worldwide. From 2014 through 2015, the proportion of cultured Neisseria gonorrhea isolates that were resistant to at least one antibiotic rose from 52% to 60%, with increases observed in the proportion of isolates resistant to azithromycin (from 1.3% in 2010 to 4.7% in 2015) and in the proportion of isolates with decreased susceptibility to the cephalosporin antibiotics cefixime or ceftriaxone (from 1.1% and 2.7% in 2014, respectively, to 1.9% and 3.5% in 2015).
Since 2001, the rate of gonorrhea infections in Canada has more than doubled. But the country has not yet reported any treatment failures resulting from resistance to azithromycin and decreased susceptibility to cephalosporins—the currently recommended dual therapy for gonorrhea.
On a positive note, the CARSS-2017 Report showed that the rate of healthcare-associated Clostridium difficile infection (CDI) in Canada continued to decline, falling from 6.64 cases per 10,000 patient-days in 2015 to 4.05 cases in 2016. Surveillance of sentinel hospitals beginning in 2015 showed that 37% of all CDI reported in patients admitted to those hospitals was community-associated.
Reductions in human, animal antibiotic use
The CARSS data also show some encouraging trends in antimicrobial stewardship, particularly in community antibiotic use.
Overall, an estimated 22.6 million antibiotic prescriptions were dispensed in Canada in 2016, with a total expenditure of nearly 700 million Canadian dollars. Analysis of human antibiotic use in the community, which accounted for 92% of all antibiotic prescriptions dispensed in the country, showed that the rate of prescribing dropped from 18.3 defined daily doses (DDDs) per 1,000 inhabitant-days in 2012 to 17.4 DDDs in 2016. Amoxicillin (25% of prescriptions) and azithromycin (10%) were the most frequently prescribed antibiotics in 2016.
Family physicians accounted for 65% of all antibiotic prescriptions dispensed through community pharmacies, most frequently for respiratory infections, genitourinary system infections, and skin and other soft-tissue infections. Data from 2015 showed a downward trend in the antibiotic prescribing rate of physicians and a stable rate for dentists.
When Canada's community antibiotic consumption in 2015 was compared with 2015 data on outpatient antibiotic consumption in Europe, Canada ranked 13th of 31 countries (ranked from lowest to highest consumption). In 2014, Canada ranked 12th. Europe is considered a good candidate for human antibiotic use comparisons to Canada, because the European Surveillance of Antimicrobial Consumption Network is one of the largest standardized data sources on human antibiotic use and employs methods similar to CARSS's.
The proportion of antibiotic doses in Canada purchased for use in the hospital also remained steady, at around 8%. Of note, however, was an increase in 2016 in hospital purchasing of daptomycin, a last-resort antibiotic generally reserved for life-threatening S aureus and Enterococcus infections.
In addition, the report shows a first-time decline in the amount of medically important antibiotics sold for use in animals. In 2016, the volume of medically important antibiotics distributed for use in food-producing and companion animals in Canada was 1.0 million kilograms—17% lower than in 2015. This decrease was highlighted by a 56% drop in the quantity of fluoroquinolones distributed for use in animals. Of these antibiotics, 99% were used in food-producing animals.
Compared with the 31 European countries that provide data to the European Surveillance of Veterinary Antimicrobial Consumption, Canada ranked fifth-highest in animal antibiotic consumption measured as milligrams of drug per kilogram of animal.
The CARSS-2017 Report also identified several gaps that need to be addressed to improve the depth and the quality of the surveillance data. These include limited data on antibiotic-resistant organisms in the community, non-academic hospitals, and long-term care facilities, and no or limited data on the appropriateness of the antibiotics that are prescribed. In addition, farm-level data on antibiotic use in animals are limited to sentinel farms in swine and poultry.
The PHAC says it will implement a number of initiatives over the next several years to enhance surveillance data in hopes of improving the country's ability to respond to antimicrobial resistance threats.
See also:
Nov 10 CARSS-2017 Report executive summary