The results of a randomized clinical trial conducted in Kenya show that taking a dose of the antibiotic doxycycline after unprotected sex did not significantly reduce the incidence of sexually transmitted infections (STIs) in cisgender women, but many who were supposed to take the drug might not have, researchers reported today in the New England Journal of Medicine.
The findings are in stark contrast to previous trials conducted in men who have sex with men (MSM) and transgender women that have found that doxycycline postexposure prophylaxis, or doxy-PEP, significantly reduced STI incidence. But the investigators say that the results likely reflect low adherence to the intervention among trial participants.
STIs not significantly lower in doxy-PEP arm
In the trial, which was conducted from February 2020 to October 2022, a team of US and Kenyan investigators enrolled and followed Kenyan women ages 18 to 30 who were not pregnant and were receiving HIV pre-exposure prophylaxis (PrEP). Participants were randomized 1:1 to receive 200 milligrams of doxycycline hyclate within 72 hours of condomless sex, plus quarterly STI testing and treatment, or standard care (quarterly STI testing and treatment alone).
The investigators followed up on the participants over 12 months, collecting hair samples quarterly for objective assessment of doxycycline use. The primary end point was any incident infection of chlamydia, syphilis, or gonorrhea.
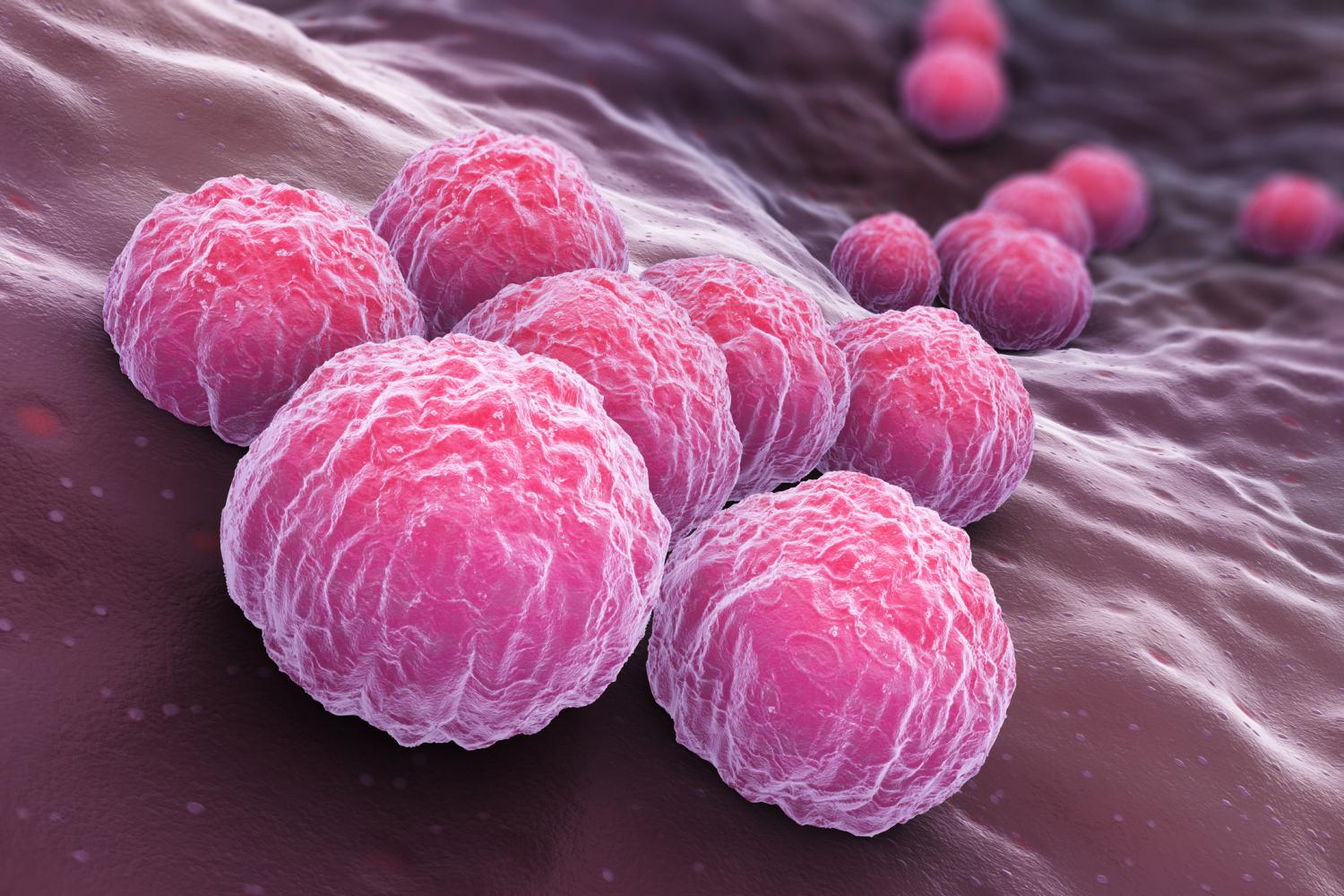
A total of 449 participants were included in the study, with 224 assigned to the doxy-PEP group and 225 to the standard-care group. Overall, there were 109 incident STIs—50 in the doxy-PEP group (25.1 per 100 person-years) and 59 in the standard-care group (29.0 per 100 person-years). The overall quarterly incidence of STIs wasn't significantly lower with doxy-PEP than with standard care (relative risk, 0.88; 95% confidence interval [CI], 0.60 to 1.29). Chlamydia accounted for 85 of the 109 confirmed STIs (35 in the doxy-PEP group vs 50 in the standard care group).
The results of subgroup analyses of STI incidence according to age, use of contraception, history of transactional sex, and STI detection at baseline showed results similar to the primary analysis.
Many might not have actually taken doxycycline
But while participant-reported adherence in the doxy-PEP group was moderately high, among the 50 participants randomly selected for evaluation of doxycycline concentrations in hair, the investigators detected doxycycline in only 58 of 200 visits (29%). That finding, the study authors say, suggests that 44% of the participants in the doxy-PEP arm may not have taken the antibiotic.
"Low detection of doxycycline among participants assigned to receive doxycycline PEP offers a primary explanation for the differing results between this trial and other studies of doxycycline PEP," they wrote. "Adherence is a necessary component of effective medical interventions when under individual control."
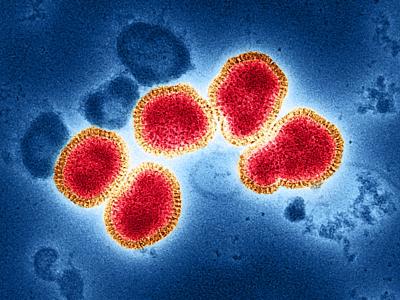
In contrast, in the DoxyPEP trial, which included MSM and transgender women with a history of STIs in San Francisco and Seattle, 86% of participants in the intervention group reported taking doxycycline consistently. The results of that trial showed that participants in the doxy-PEP arm saw incidence of chlamydia, syphilis, and gonorrhea fall by 88%, 87%, and 55%, respectively.
Low detection of doxycycline among participants assigned to receive doxycycline PEP offers a primary explanation for the differing results between this trial and other studies of doxycycline PEP.
Those results led the Centers for Disease Prevention and Control to develop guidance for use of doxy-PEP in MSM and transgender women. A draft of the guidance was released in September for public input, and a finalized version will likely be released next year.
The study authors also suggest that the results may be influenced in part by the high prevalence of tetracycline-resistant gonorrhea in Kenya, which could explain the lack of efficacy in preventing Neisseria gonorrhoeae infections in the trial. In addition, they point out that the incidence of syphilis in Kenya is low.
They say the results emphasize the need to provide effective and acceptable STI prevention options for women, who bear the highest global burden of STI complications.
More research needed into pharmacodynamics
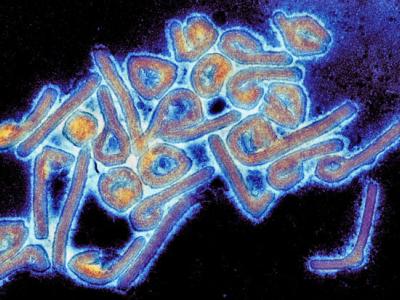
In an accompanying editorial, Jeanne Marrazzo, MD, an STI expert and director of the National Institute of Allergy and Infectious Diseases, says the results are disappointing given the efficacy that's been documented in other populations, the "relentlessly increased" incidence of STIs in the United States and around the world, and the lack of vaccines for STIs on the horizon.
Marrazzo suggests that further research is needed into whether the pharmacodynamics of doxy-PEP work differently in cisgender women, who more commonly have endocervical infections than rectal or pharyngeal infections, and into reasons why doxy-PEP adherence may be lower in this population.
"For chemoprophylaxis against STI, we need to do better in working out the science of drug delivery, the motivation and context for product use, and the background antibiotic susceptibility to inform the design of interventional trials," she wrote. "With women bearing the brunt of the long-term consequences of untreated STI, we owe them no less."