A large study yesterday by researchers at the University of Pennsylvania has found a dramatic increase in cases of multiply recurrent Clostridium difficile infection (mrCDI).
In the study, published in the Annals of Internal Medicine, a retrospective examination of data on more than 38 million patients from a large nationwide insurance database showed that, from 2001 to 2012, the annual incidence of mrCDI jumped by 189%—more than four times the rate of increase in initial cases of CDI.
The authors of the study say the reasons for the dramatic increase, seen across the country, are unclear.
'Excessive increase' across entire US
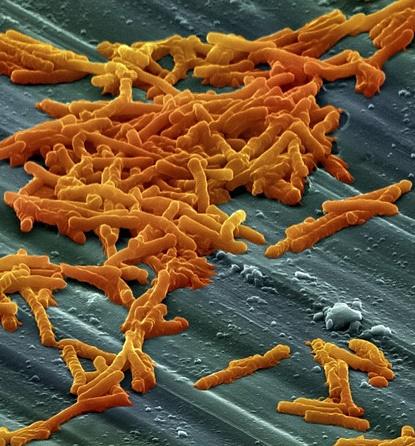
C difficile, a common environmental bacterium that can survive routine environmental cleaning in hospitals, causes inflammation of the colon and severe diarrhea. CDI is the most common healthcare-associated infection in the United States, responsible for about half a million infections and 29,000 deaths in 2011, according to the Centers for Disease Control and Prevention (CDC). It costs the US healthcare system roughly $5 billion a year.
CDI mainly affects older patients who are taking antibiotics for other infections. The antibiotics disrupt the normal gut flora, wiping out the good bacteria and allowing C difficile to flourish in the intestinal tract. And CDI can be tricky to completely cure, partly because treatment requires more antibiotics and further disruption of the gut microbiome.
At least 20% of patients who get an initial CDI have a recurrent infection within 8 weeks, with the risk being as high as 50% to 60% after three or more infections. In addition, recurrent CDI is associated with higher morbidity and mortality.
But while the rise in CDI over the past two decades has been widely reported, as yet it's been unclear how big a problem recurrent CDI, particularly mrCDI, presents for the healthcare system.
To get a better understanding of mrCDI incidence, the researchers, from the University of Pennsylvania's Perelman School of Medicine, analyzed records from 38,911,711 commercially insured patients in the OptumInsight Clinformatics Database, which captures medical and pharmacy claims data. They defined mrCDI as a case that was treated with at least three courses of CDI antibiotics (oral or intravenous metronidazole, oral vancomycin, or oral fidaxomicin), with each course at least 14 days and no more than 56 days after the start of the last antibiotic course.
Overall, the researchers found that 45,341 patients in the database had at least one episode of CDI from 2001 to 2012, with 1,669 of those patients (3.7%) having mrCDI. The median age of the CDI patients was 46 years, and 58.9% were female. Over the course of the study, the annual incidence of CDI rose by 42.7%, from .4408 to .6289 cases per 1,000 person-years. The annual incidence of mrCDI jumped by 188.8%, from .0107 to .0309 cases per 1,000 person-years.
"This excessive increase in incidence of mrCDI was independent of other known risk factors for CDI and occurred across all regions of the United States," the authors write.
A follow-up analysis of the CDI patients found that patients who developed mrCDI, when compared with those who had only one episode, were more likely to be older (median age 56 years vs. 49 years; adjusted odds ratio [aOR] per 10-year increase in age, 1.25) and female (63.8% vs. 58.7%, aOR 1.24). In addition, they were more likely to have used antibiotics (72.3% vs. 58.8%, aOR 1.79), proton pump inhibitors (24.6% vs. 18.2%, aOR 1.14), and corticosteroids (18.3% vs. 13.7%, aOR 1.15) within 90 days of CDI diagnosis. Diagnosis in a nursing home (2.1% vs. 0.6%, aOR 1.99) and chronic kidney disease (10.4% vs. 5.6%, aOR 1.49) were also associated with increased risk.
Although these factors are linked to increased risk of mrCDI, the authors say it remains unclear what's causing the observed increase in recurrent infections. Even after adjusting for these potential confounders, they note, the odds of developing mrCDI increased by roughly 8% per year.
They suggest one possible cause could be the emergence of the North American pulsed-field gel electrophoresis type 1 (NAP1) strain of C difficile. Studies have found that NAP1, which is resistant to fluoroquinolone antibiotics, is associated with greater odds of severe disease and lower clinical cure rates than other C difficile strains, making it a factor in recurrent infections.
Limited treatment options
More important, the authors suggest, the dramatic increase in mrCDI incidence means demand will rise for therapies to treat recurrent infections, which are more difficult to treat and have limited options.
Fidaxomicin, an antibiotic with a narrow spectrum of antimicrobial activity compared with other antibiotics used for C difficile, and bezlotoxumab, a human monoclonal antibody that can be added to standard antibiotic treatment, are two newer options. In clinical trials, patients taking these drugs have had lower rates of recurrent infection. But both drugs are expensive.
Another option is fecal microbiota transplantation (FMT), a procedure in which fecal matter from a healthy donor is mixed with saline and placed in a sick patient. The idea behind FMT is to restore the beneficial gut bacteria that have been suppressed by antibiotics. Studies have shown high rates of success for FMT in patients with recurrent CDI, but wider use of the procedure has been hampered by several factors, including availability and screening of donors. In addition, there has been little research into long-term effects.
"While we know that fecal microbiota transplantation is generally safe and effective in the short term, we need to establish the long term safety of this procedure," lead study author James Lewis, MD, MSCE, a professor of gastroenterology at the University of Pennsylvania, said in a university press release.
Lewis and his colleagues say they hope this study will lead to further research that could guide optimal treatment for mrCDI.
Sameer Saini, MD, MS, and Akbar Waljee, MD, MSc, authors of an accompanying editorial, agree. "A better understanding of the epidemiology of mrCDI is a critical first step toward developing a sound strategy to address this growing public health challenge," they write.
See also:
Jul 4 Ann Intern Med study
Jul 4 Ann Intern Med editorial
Jul 3 University of Pennsylvania School of Medicine press release