Use of a rapid polymerase chain reaction (PCR) test in patients with infectious diarrhea did not reduce antibiotic use compared with stool culture, researchers reported today in Antimicrobial Stewardship & Healthcare Epidemiology.
To evaluate the impact of multiplex stool PCR testing versus stool culture on antibiotic use in patients with infectious diarrhea, researchers from Baylor College of Medicine evaluated data on hospitalized adult patients with suspected infectious diarrhea during two periods: the preintervention period, when stool cultures were routinely collected from patients, and the postintervention period, when all orders for stool cultures were converted in the electronic health record (EHR) to multiplex stool PCR tests. The primary outcomes included antibiotic days of therapy (DOT) and length of therapy (LOT).
In the preintervention group, stool cultures were negative in 71 (94.7%) of 75 patients, compared with negative stool PCR panels in 58 (71.6%) of 81 patients in the postintervention group. There was no meaningful difference in DOT and LOT between the two groups. In both groups, the median DOT and LOT were 0 days, with ranges of 0 to 10 days (DOT) and 0 to 5 days (LOT) in the preintervention group and 0 to 8 and 0 to 5 days in the postintervention group. Similarly, the incidence rate ratios for DOT (0.71; 95% confidence interval [CI], 0.42 to 1.22) and LOT (0.67; 95% CI, 0.36 to 1.24) indicated no change in the incidence rate after the intervention.
Findings might not be generalizable
The study authors note that other research on multiplex stool PCR tests, which have much faster turnaround times than stool cultures, has produced different outcomes, and that the small sample size of the study, and their institution's existing culture of antimicrobial stewardship, could diminish the generalizability of the findings.
"Future research investigating the impact of stool PCR testing on antimicrobial use may help inform clinical decision making or the development of clinical decision-support tools within EHRs," they wrote. "As antibiotic stewardship becomes increasingly essential with the advent of drug-resistant pathogens, diagnostic stewardship must be considered in patient evaluation and treatment, including the turnaround time and result sensitivity."
Diagnostic stewardship must be considered in patient evaluation and treatment.
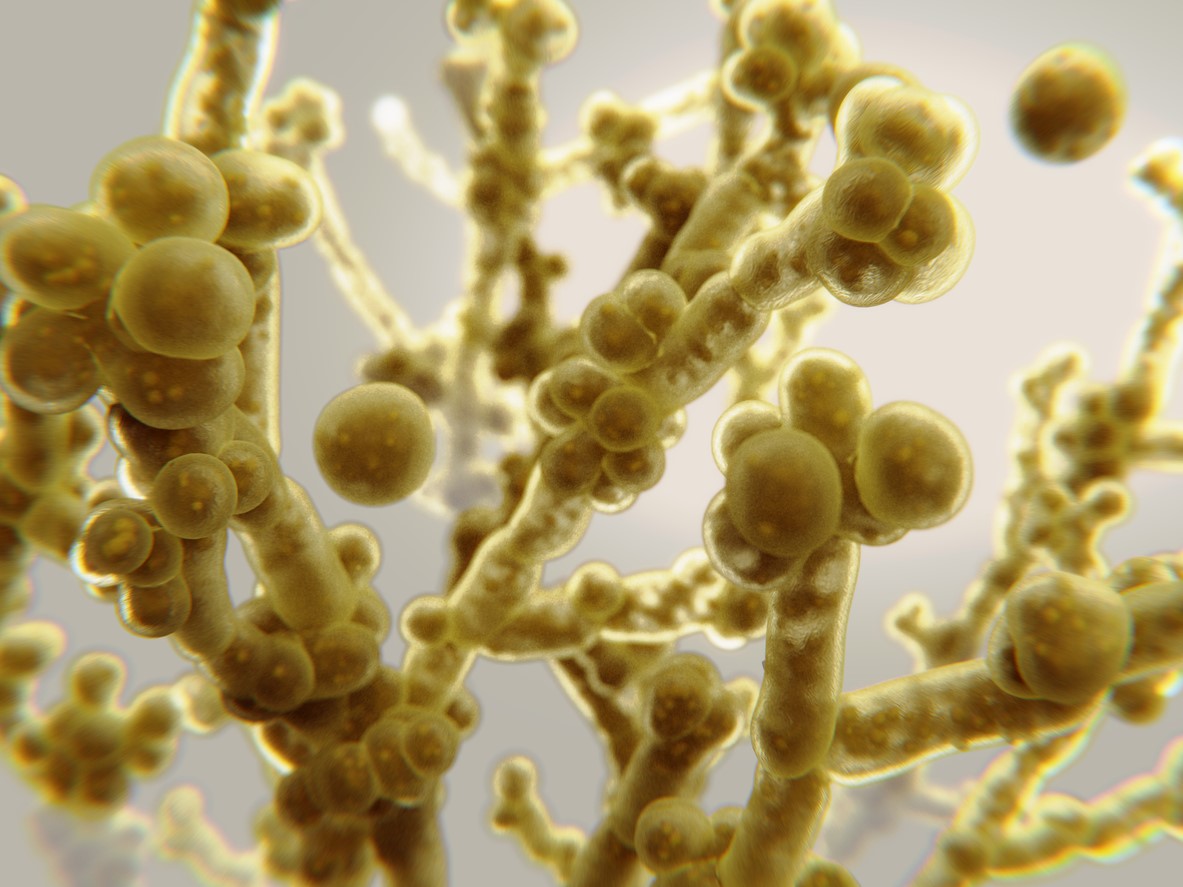 Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology.
Testing by a team of researchers with the Louis Stokes Cleveland VA Medical Center indicates that sporicidal disinfectants are more effective against the multidrug-resistant fungal pathogen Candida auris than quaternary-ammonium disinfectants, according to a study published today in Infection Control & Hospital Epidemiology. The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an
The risk of flu-related intensive care unit (ICU) admission was sevenfold higher in lower middle-income countries (LMICs) than in high-income countries (HICs), according to an 














